I had the ExoVasc procedure on the 8th December 2008, aged 26. I’ve been aware of Marfan’s Syndrome since childhood, although not particularly well aware of its implications for the aorta. My older brother died from aortic dissection in 2003, and after subsequent monitoring I was referred to Bristol in July 2008 as my aorta continued to dilate and surgery looked increasingly necessary. I was made aware of the ExoVasc procedure by the surgeon, and of the alternative, which for me would be valve-sparing surgery. I chose to, at the least, find out more about the ExoVasc. This involved a few outpatients’ appointments at the Brompton, and a couple of separate MRI scans, between July and October 2008.
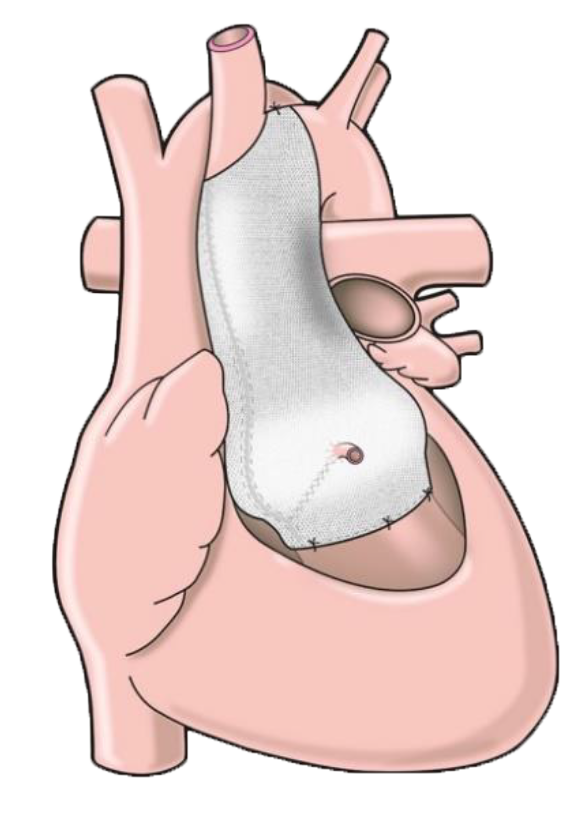
There were obviously other important grounds on which to base an ExoVasc vs. conventional surgery decision than, simply, the severity of the procedure. However, the more I learned about the ExoVasc the less of a decision it really became. I much preferred the idea of the ExoVasc to replacing large amounts of tissue; I was also aware that it posed lower constraints on subsequent surgery; and once I’d decided that the ExoVasc appeared to be the best option, being a less severe operation obviously reduced my inevitable concern.
The procedure took place on Monday 8th December, in the morning, after a visit from Professor Pepper. I don’t have much memory of what happened directly before the operation. I remember waking up on Monday afternoon and spending the night in intensive care, not feeling in pain or much discomfort, just very narcotised after the anaesthetic.
On Tuesday 9th I was transferred to the High-Dependency Unit, and in the evening I had some visitors. The nurses at the Brompton really were fantastic. I stayed in the HDU until Thursday, due to a slight temperature and higher-than-ideal levels of CO2 in my lungs; I also had no appetite. Whether it was simply that time passed or that I stopped taking morphine, I felt much better by Thursday and had regained my appetite by Friday morning.
Two things that caused me discomfort in hospital were not sleeping well due to only being able to lie on my back (this passed after maybe five days) and the twice-daily subcutaneous injection of Heparin (anticoagulant). Not everyone is given this drug, and I didn’t notice anyone else finding it painful, but if you do, as I did, the least-painful place I found to have it injected was underneath the shoulder, towards the back of the arm. Relative to what the procedure involves, these discomforts are decidedly minor.
I was discharged on Sunday 14th, a week after being admitted; I made the 2-hour train journey home, and was very grateful for my girlfriend being with me! The journey was no problem, but I wouldn’t have liked it to be any longer. It’s now about six weeks since the operation and I’m feeling good, just taking lower-than-pre-op doses of a beta-blocker and ACE inhibitor. I’m back to normal activities, the only thing I can’t do is lift heavy things due to my healing sternum, which is not a problem around the house.
I was visited by Tal on the Wednesday while I was still in hospital, the first time I’d met him – now knowing the history of the operation, it seems difficult to acknowledge here the massive thanks that I and hopefully many more to come will owe him, Professor John Pepper, and everyone else involved. The procedure is an opportunity, and whatever the future holds I’ll remain thankful for it. My only concern remains that potential patients might not be aware of the existence of the procedure as an alternative.