My name is Scott; I am 40 years old and come from Glasgow. I was given a “putative” diagnosis of Marfan Syndrome in my early thirties after being assessed against the Ghent criteria (6’5’’ tall at 14, painfully thin, arachnodactyly, flat feet, pectus carinatum, etc). However, further genetic testing did not reveal any evidence of the much touted fibrillin gene mutation that is being claimed as the definitive cause of the condition. Where does that leave me? Somewhere out in the “Marfanoid” nowhere land with a heck of a lot of other people, I guess.
What I definitively did have were signs of aortic root dilation which were to be monitored via six monthly MRI scans. My first measurement was 4.5cm; still well below the magical 5cm mark where surgical intervention starts becoming a necessity. Being asthmatic, I was prescribed Losartan, in place of the more usual Beta Blockers, to help reduce the workload on my heart – simultaneously, Losartan itself was being clinically trialled to assess whether it provably slowed the progression of aortic root dilation in humans (as it seemingly did in mouse models). I was hopeful that this would work for me – like anyone else, if I could somehow get away from this thing without undergoing any heart surgery at all, that would be the ideal fantasy scenario, right?
However, real life intervened. My measurements crept up little by little, seemingly every year, until I was up around the 4.9cm mark… surgery really was going to happen, sooner rather than later. Better sooner, I thought, while I’m still young-ish and fit-ish. My local hospital offered either the traditional Bentall procedure or their preferred option of valve sparing surgery (the “David” procedure). Neither was particularly appealing to me. The former has the well known downside of the lifetime of Warfarin quaffing with the severe lifestyle curtailment that will probably bring. The latter option offered an (initial) escape from the rat poison but brought with it the prospect of a long, difficult surgical procedure of its own… and, worse, the very real prospect that the “fix” would only last ten or fifteen years and that I would eventually have to go in and get a second operation in my latter years where the Bentall procedure would have to be applied to me anyway. There must be a better bet out there, I thought…
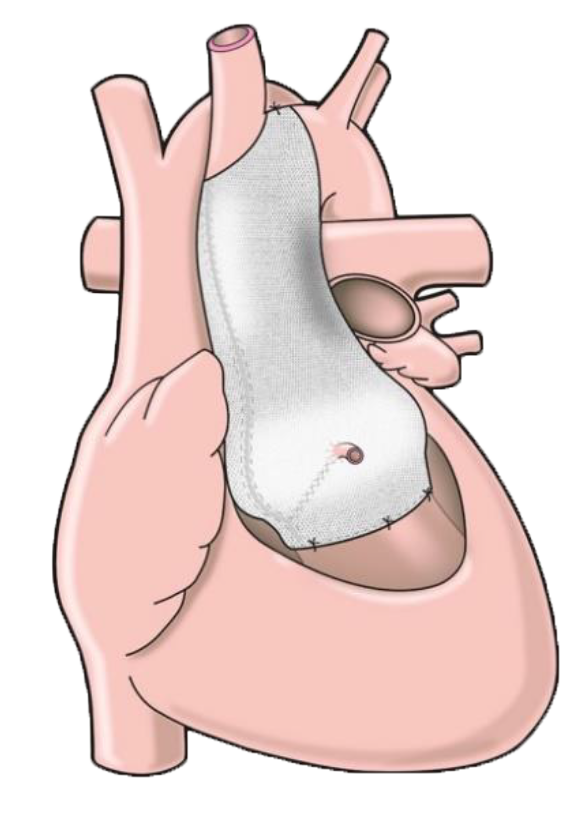
In my desperation to seek alternatives to the rocky path I seemingly had laid out before me, I was lucky enough to stumble upon an interview with Tal on the internet discussing the PEARS approach and it made immediate sense to me. The details were compelling: a bespoke support device to stop the aortic root dilating whilst simultaneously strengthening it; a relatively straightforward, two hour operation, no heart-lung machine required; no endless prescription of Warfarin post-op; the distinct possibility of the procedure being a one-shot, lifetime lasting deal. Furthermore, the man himself had his own skin in the game and if it was good enough for him to have it done upon himself, it was certainly good enough for me – where do I sign up?
Of course, this is where the fun starts. It’s a brand new technique, still in its infancy, they said. There’s not enough data available, they said. Well, every emergent innovation in every field of science starts off as a brand new technique with a limited data set. That data set will forever stay limited if you stop people from adding themselves to it. Besides, as a young-ish single man with no children, I am exactly the kind of candidate for doing this kind of thing. I didn’t view it as a risk – the concept of the device is pretty clear, even to a lay person, so I knew what I was getting into. If there was to be a problem during the operation (a tiny 2% chance), I would simply get fitted with the Bentall device – definitely plan B but better than the alternative. The potential upside was far too good for this to bother me in any way. Bring it on!
After a fair bit of to-ing and fro-ing, and with the excellent support of my cardiologist in Glasgow, Dr Hamish Walker, and my local GP, Dr Susan Perryer, I was able to meet the surgeon, Mr Mario Petrou, at the John Radcliffe Hospital in Oxford for my initial face to face discussions in January of 2013. We had an immediate rapport as it was clear from our dialogue that he saw exactly why I wanted to go down the PEARS route and what I was hoping to achieve from it. The conversation only further cemented my desire for this procedure to actually happen to me.
My operation took place in the first week of August. The procedure was performed on Monday August 5th and I was sent home on Saturday August 10th. It was remarkably straightforward and uneventful. Much of this must be credited to the wonderful skills of Mr Petrou, to whom I am eternally grateful. Furthermore, the level of care offered by the nursing teams on both the Critical Care Unit and the Cardiothoracic Ward at the John Radcliffe was little short of magnificent. Tal himself came in to see me on the Wednesday and was full of enthusiasm and positive vibes. I struggled to express how thankful I was for his marvellous invention – I still couldn’t quite believe how smoothly things had gone for me. During the week, I had a couple of small bouts of sickliness via a couple of hours of both pericarditis and tachycardia but nothing to frighten the horses. I was alive and had a future again.
Post discharge, I returned to Scotland to stay with my wonderful brother and sister-in-law, Matt and Elaine, for a fortnight while I recovered my energy. Genuinely, pain was only a very small problem indeed (discomfort is a better word, really). The biggest initial issue was tiredness and general fatigue. It really does take a lot out of you. However, I can only imagine that this process would have been so much more difficult if I was recovering from either of those other two, more onerous, surgical procedures that were on offer before the PEARS approach became available to me. And, what’s more, I don’t have to take any of that bloomin’ rat poison, either…