I have two daughters aged 20 and 18 who also have Marfan.
July 2004
Annual echo at St George’s. My aortic root measurement is apparently now 4.8cm. This is a rise of 0.2mm from the 4.6cm of the last few years. By coincidence, both my daughters’ measurements appear to also be 4.8cm. Discussion with my geneticist Dr Child suggests that surgery options should at least be considered. Quite scary, particularly when thinking about the girls.
My brother Martin had aortic replacement surgery 9 years ago. He has a tin valve fitted and will be on Warfarin for the rest of his life. At 56 he is very fit, rides his bicycle daily and is more active than his peers. I watched him recover from his op and was astonished at his progress. I personally do not wish to take rat poison for the rest of my life, and think somehow that a tin valve that I could hear would probably send me nuts.
September 2004
Together with my eldest daughter, I attended Guy’s for an appointment with a leading heart surgeon. She explained that by having the op done early, whilst fit and healthy, there was a chance that my natural valve might be spared. No decision could be made until I was under the knife though, and most ops seemed to end up with artificial valves fitted. My daughter and I immediately realised we equally shared huge levels of cowardice. We also both reflected on how fantastically fit and healthy we currently felt and mutually decided that our dilemma was thus: whether to act now and hope for valve sparing, or trust to medical progress and hope that some great new breakthrough might just be around the corner. Cowardly optimists both, we recklessly gambled our all on the latter course deeming we were strong enough to carry on a while.
January 2005
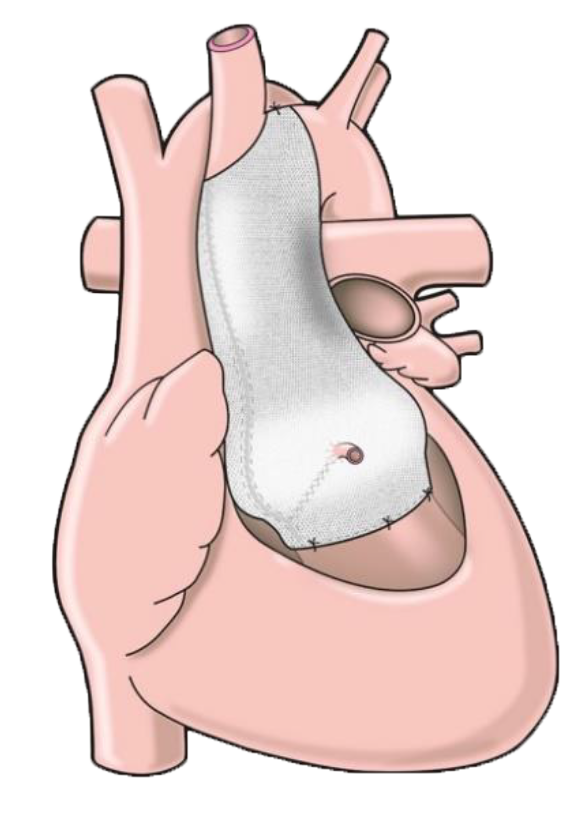
My brother Martin presented me with an abstract from the Lancet entitled something like “The Tailor of Gloucester, a jacket for the Marfan’s Aorta” The eminent surgeon who had performed Martin’s operation, Professor Tom Treasure, was giving obvious support to a procedure invented by an engineer who had Marfan, Tal Golesworthy.
In short, this brilliant engineer, with a wealth of experience in the dynamics of viscous liquids moving around pipework, had used his engineering know-how to solve his own problem. Some of the established medical profession proved remarkably difficult to convince that another discipline could be used to solve one of their problems, but with his tenacity, and the great support of enlightened minds such as Professor Treasure’s, Mr Golesworthy continued crashing through roadblocks to invent the prototype, raise the funding to make it all possible, and finally act as the first guinea pig for this untested process. This was a terrific story of modern day true grit and unstoppable determination. It was also, quite literally, possibly the answer to a prayer. I emailed both Tal Golesworthy and Tom Treasure, and was delighted to receive two speedy and positive responses: “Next step, contact Professor Pepper”, he who had fitted the first ever ExoVasc to Tal Golesworthy. I duly made arrangements to be referred.
Professor Pepper gave me a quick and positive reply. Clinical trials were to take place, and if suitable, I could be included. An appointment was fixed for 24 March 2005.
I spent time researching what I could about the ExoVasc, and the team involved. The academic records of the team members proved rapidly awe-inspiring. I quickly realised that if I were lucky enough to be entertained by these people at an early stage demonstrating their new process, I could not be in better hands, anywhere, worldwide.
In addition, Tal Golesworthy proved to be the most affable guy imaginable. He provided me with loads of background information as well as the humorous anecdotes and his specific scientific theorem. We shared youthful interest in motorcycles, and, I like to think a positive attitude to life. I could not easily express how much I admired his tenacity in pushing on through all the barriers to make this possible, not just for me, but for my daughters, and everyone else who might benefit. Tal is just far too modest to recognise quite how profound the effect of his work is to us, but I would say without hesitation that it is one of the greatest advances in this generation for the Marfan community.
24 March 2005
Appointment with destiny. Professor Pepper, having studied my previous echo tapes explained the process, seemed pleased that I was quite familiar with it, and pronounced that if I was willing, we would press on and get it done ASAP. An MRI scan was ordered, with the ExoVasc to be produced and fitted approximately four weeks later. I left hospital somewhat shocked, and, with my nephew, immediately proceeded to get roaring drunk down Kings Road, because we could!
As the hangover receded the next day, I started to get fit ready for surgery in earnest.
During the period between this appointment and the MRI scan, my wife attended St George’s with my two daughters for their annual echo. I have included this, because it was the wise counsel of Dr Child that properly prepared and helped my wife Christine accept the benefits of this course of action. I am famous for jumping in with both feet, full of enthusiasm and generally leaping up and down where angels fear to tread. Christine had genuine concerns and Dr Child discussed in full the options and advantages and did a wonderful job of laying those concerns to rest. Indeed, my daughters are now quite comfortable with the idea of undergoing this process themselves in the future.
19 April 2005
MRI scan at Royal Brompton Hospital. The scan depends on a relaxed patient for best clarity. Suitably armed with a soothing Simon & Garfunkel CD I settled down inside the space age tube for about 40 minutes being instructed variously to breathe in, out, and hold my breath. The scan process made some odd noises, but that was all there was to it.
13 May 2005
Second MRI Scan at RBH, prior to being admitted. Exactly the same procedure as before.
15 May 2005 (Sunday)
Admission to Princess Alexandra ward for operation the following day, Monday 16 May 2005. Having spoken to both Tal and my brother Martin, I suggested Christine stayed down in Dover until Tuesday. I knew I would be sedated and in Intensive care until then, and would neither have a care in the world nor probably recognise her until this time.
Sunday spent undergoing usual checks, X-Rays and blood-letting sessions from the Vampire Squad. The anaesthetist gave detailed information, and I became immediately aware of the fantastic staff that work in the ward. I also made some good friends, all patients preparing to undergo ops the next day or their families. As I settled down to eat a very pleasant tea, Professor Pepper himself appeared! I thought that one as eminent as he would surely be at home in the bosom of his family, having a much needed break at the weekend, but, no, here he was telling me all about what to expect the next morning, and advising me that I was to go first. This single detail made me feel both special and important and filled me with great confidence. The small amount of research I had done told me that even if it all were to go pear-shaped, you could not wish a better man present. Together with my new shipmates, we found amusement in the next ritual, that of shaving off most of our body hair. Thence to bed, awaiting the dreaded “Nil by Mouth”, the ceremonial early shower and perhaps hoping that the pre-med would be every bit as good as promised. Zzzzzzzzz.
16 May 2005 (Monday)
Up at 05.45 and drank as much water as possible before cut off at 06.00hrs. Showered, and put on that most uniquely unfashionable of all garments, the gown with one button at the back. Pre-med at 07.00hrs. Every bit as good as promised, chuckling to myself and phoned home to reassure Christine that I was feeling positive and “good to go.”
Just before 07.30, the press gang arrived and I was taken down to theatre. The anaesthetist kept me well informed, and warned me that I would wake up with a tube in my mouth and down my throat and neither to panic nor gag when discovering this. It was confirmed that Professor Pepper was present and with a certain knowledge that I was surrounded by a highly competent bunch of top professionals, I slipped into my dreams.
Sometime in the afternoon I became conscious again. I was in Intensive Care. I felt no pain, and I was immediately aware that the staff were paying close attention to me. As promised, I gagged on the horrid tube going down my throat. It wasn’t long before I was prepared for its removal. I was instructed to give a long cough as it was extracted, and that was probably the most unpleasant part of the whole process, but so liberating to be free of it. My nursing back to the point of being a human being was made delightful by the wonderful administrations of the team. With the clear potential to be a frightening and confusing time, my memory of this period was of real genuine warmth and support throughout by close personal friends. It was quite exceptional. Also during this time, I was delighted to find that I had been very thoroughly painted an apparently indelible bright pink, and an attempt was made to put shocking white tights on me. With tacit and covert support from my nurse I was advised that it would be no problem if I refused this indignity. I did, and felt much better for being a rebel!
17 May 2005 (Tuesday) morning
One minor problem was causing the staff concern, that of fluid retention. I had a large drip giving me intravenous fluids, and was taking good sips of water, but very little was coming out. This situation was being mentioned in high places, until I had a cup of NHS tea. With sudden and dramatic effect, this problem was reversed, establishing a routine of exploding catheter bags over the next 36 hours worthy of an old “Carry on” film. I was quick and indeed eager to resume eating all available food, but remained in Intensive care for about 24 hours, during which time the physiotherapist made her first visit and made me fully inflate my lungs for the first time. This was a bit painful, and I had been supplied with a self-dosing morphine button that was useful at this stage. The lungs had been partially collapsed, and it was explained that like a balloon being blown up, the first big puff was the hardest. It was, and got progressively easier after this. Throughout my time in Intensive care, I had a small nose tube puffing out extra oxygen, and I was most comfortable, and attended with the greatest possible care. I was also kept closely informed every time a friend or family member called.
17 May 2005 (Tuesday) afternoon
At about 14.00hrs I was deemed fit to return to the high dependency unit on the ward. I was duly wheeled up to be greeted by my wife Christine, brother Martin and his wife Jo. I was in fine spirits, and I could tell they were surprised to see this. I was ragged for having been painted pink, and Martin had quickly got hold of the story of the exploding catheter bags and combined it with my notorious lack of success with DIY plumbing projects, pointing out to the assembled professionals that any venture involving me with said plumbing was doomed to failure. Great to see the family again, great to reassure them that all was OK. After a couple of hours my brother took his leave, and I was pleased to have the company of Christine all to myself for a while. I managed to get up and walk to the bathroom for a wash and with her assistance, together with two trolleys one for an oxygen cylinder, and one for the assorted drips. I requested to be allowed to do this, but the nurses were very happy with it, because they like to bully a patient back up on their feet ASAP. (I privately also wished to prove to myself that I would be able to manage without a bedpan when the time came.) After I had eaten dinner, at about 2100, Christine departed for her overnight accommodation at the nurses’ home, and I now felt tired and fell into a fitful doze. I knew I could not sleep easily on my back, and as I regularly do shift work I tend to have an unorthodox sleep pattern. At about midnight, the nurse came to remove the catheter. I had been a little apprehensive about this, but it was no problem at all. Another flipping tube got rid of! My fitful sleep paid dividends: having spent my awake time being as charming as possible to the lovely hard working nurses, one of them asked if I would like a delightful en-suite side ward all to myself!!!! What a result.
18 May 2005 (Wednesday)
Smugly ensconced in my luxurious new surroundings, I had the wrist intravenous contraption removed but I perhaps got a little too bold. At about 0900 I got up, threw caution together with my oxygen supply to the wind, and pranced across to my bag, fished out my wash kit and began to vigorously brush my teeth, my mouth understandably tasting of, well, perhaps we won’t go into that. Anyhow, despite the wonderfully refreshing taste, I felt a little flustered, and thought it prudent to return to bed for a rest and to plug the oxygen back in. I had a few palpitations and realised my heart rhythm was somewhat irregular. I duly informed my nurse. When Christine turned up to visit at 1000 they were wiring me up to an ECG and I was being monitored for all sorts. I then heard those dulcet tones now so familiar of Tal Golesworthy coming from outside the door. I was really pleased that he had come to see me, without him none of this would have been possible, but I felt a little miffed that I could not leap up and greet him as I wished to. I considered my current situation to be self-inflicted. Anyhow, apart from an irregular heartbeat, I felt fine and once I had been wired up I was able to greet my visitors properly. Tal and I compared our chest scars, and I think mine was deemed to be the neater of the two. His visit passed mainly as an interlude of boisterous fun, we had a mutual experience unique at this time and found it exhilarating to have survived it with so little pain or discomfort.
Tal described his recovery, and the requirements of the hospital for release. One crucial test was to walk round all four wards on the floor, and then to ascend and descend two flights of stairs. Tal, and also my brother Martin had both tried the stairs before the test to ensure success. I resolved to do likewise. We parted reluctantly, and agreed to have a few beers together at a future date. My treatment now included another drip to stabilise my heartbeat, first for 1 hour, and then another for 23 hours. I was a little miffed at this, because progress seemed to me to equate with having less tubes into my body rather than more. I guess all the medication was now making me feel a little down, and I had further problems only achieving 93% oxygen saturation as a result of not fully expanding my partially collapsed lung. I had been sitting and lying down for most of the day and needed to stand up and get mobile to get things working properly.
Once I got up, with the assistance of Christine to pull the oxygen, and me to pull the drip stand and carry the heartbeat monitor I was able to walk quite well. This was an instant improvement, the tension went, the oxygen saturation went up to an acceptable 96-97%. It was decided I no longer needed the oxygen: another tube and encumbrance gone! My spirits lifted and this was a wonderful feeling. The nurses relieved me of two more tubes, this time drain pipes that I was glad to see the back of, but whose removal I did not particularly enjoy. I was able to complete twice the distance recommended by the physio. After making myself tired, having my evening meal and bidding Christine farewell, I fell asleep. When I woke up at midnight, I could tell that my heart rate was back to normal.
19 May 2005 (Thursday)
Poor sleep after 0100hrs. I hate sleeping on my back and was getting cramps from doing so. I got up and walked down to the day room for hot chocolate as became my regular habit to the amusement of the nurses. Without the oxygen, it was much easier to have a shower. Feeling on top of the world, Christine turned up early and I had a visit from one of my best friends. There was now no stopping me, and I did several circuits of the wards opening doors for my visitors and generally showing off. I made sure I was seen by the physio so she got the idea that I was keen! My friend took Christine back home, as she had to attend to the kids, dogs, cats and other domestic issues. She phoned me up later in the evening, displaying her obvious powers of “telephony” insisting that I was under no circumstances to attempt the stairs until given permission by the physio, and that she was going to phone the ward and warn them to watch me…
I waited until 2230hrs before creeping out of the ward. I got to the stairs and eased myself into the climb. Not too much of a problem, I ascended two flights, only to realise I was on a “prohibited” floor. After gazing into a CCTV camera, my descent was, in the manner of a naughty schoolboy, considerably quicker! This excitement left me a little breathless to be honest, so I beat a hasty retreat back to bed still feeling pretty pleased with myself. Sleep again though was fitful.
20 May 2005 (Friday)
Professor Pepper was my first visitor. I don’t know how he knew, but his first question was “Have you tried the stairs yet?” When I answered in the affirmative, at least he seemed pleased. He then pointed out the fountain on the ground floor in the fresh air and recommended it to me. He also explained that a heart would generally react “with irritation” after the attentions of a surgeon wielding a knife in close proximity. This was normal, and will re-regulate itself when my circumstances had settled. He did not seem to recommend further drug or other treatment for it. This was most reassuring, and I hung on to that. I knew Christine would be late this morning, so I did a couple of four-ward circuits and had another bash at the stairs, just to make sure I could still do it. Feeling rather pleased with myself, I had just completed this, and was quite frankly looking forward to a cup of tea and a sit down, when I bumped into the physio. I told her I had done the stairs, and she looked aghast. “What, on your own?” she squealed, I nodded. “Right then let’s do it now.” Bearing in mind I had only just finished the routine, I had to go through it all again, this time with her making me talk the whole time to indicate my breathing rate. I managed it but she pushed the pace. I was now passed fit to leave on Saturday!!! No more hospital food, no more uncomfortable bed!
When Christine arrived with my daughter, I was cock-a-hoop. I took them down to the café twice, I went to get my final x-ray on foot, avoiding the annoying bossy man with his wheelchair sent to get me. Wonderful day.
I had certainly done too much. That night my rhythms all went loco and I sweated about a kilo off. I needed to come home and settle back to my life and I knew this. I had to get out of the hospital so I didn’t tell anyone.
21 May 2005 (Saturday)
Got discharged . Took a taxi to Charing Cross. It was a wonderful journey, the Changing of the Guard was taking place and London appeared full of colour. We went over one bump that made me gasp, but that was all. I felt a little vulnerable at Charing Cross, because of the crowds. I was, however, lucky that it was Cup Final day, and the train was quiet. We got home, and I was amazed that my normally boisterous and very large Standard Poodles were very careful to approach me gently. I don’t know how they knew, but they did. Thankfully, in the evening after relaxing for a while, and the best meal of my entire life, liver and bacon, cooked in red wine, my heart rhythm went back to normal. I had a much better sleep.
22 May 2005 (Sunday)
Got up, felt marvellous. I went out on my own to walk and breathe the sea air. I set myself a target walk, but having done that, I felt more invigorated. I continued at an easy pace to do five times that distance, and also up a long slope. I came home, Christine was still asleep, so my daughter and I did washing up and cleaned the kitchen. My eldest daughter arrived, and burst out laughing, wondering who was actually the patient!
The rest of my recovery has been fast, furious and fantastic. I covered much more distance each day. The second night I managed to sleep for a while on my side, and after the first week I was back to hill walking with my dogs. After three weeks I was suffering horrendously from boredom. My brother came over and took me to France. At four weeks I went out and booked a surprise last minute holiday to Malta for myself and Christine. She had been fantastic, and far more worried than me. We had a wonderful time revisiting old haunts and taking long waterfront walks. I even had a few beers and enjoyed lovely Mediterranean food.
At six weeks I could finally drive again, and celebrated with a thousand mile marathon down to Gloucester to see my brother and also, most rewarding, to go and have dinner with the only other ExoVasc, and inventor of it all, Tal Golesworthy. I then went on to Wales for my best friend’s wedding, back to Gloucester for RAF Fairford Air Show and thence to visit family not seen in ages.
On 14 July I had another check up with the team, and when my sick note runs out, most alarmingly they have indicated I must return to work.
I would recommend this surgery without hesitation to anyone suitable. It allows for non-intrusive surgery, saving the valve and, most importantly, leaves no need for drug therapy afterwards. The team involved, especially Tal, has pushed the boundaries, fought against convention and driven progress unequalled in my generation. I am doubly pleased that through his efforts my children will be likely beneficiaries avoiding the conventional and, to me, very scary operation.
PS: Now in 2008, my two daughters have had the procedure, both are living the fullest possible lives. My life is lived at 100%, and I wonder how all those non-ExoVasc-ialists could ever keep up.
Thank you Tal. Thank you Professor Pepper and team. We as a family have been truly, truly transformed in the most positive way, both physically and emotionally. As a parent with Marfan’s I have experienced what would with biblical reference, be known as a miracle.
Peter Barker, 13 February 2008