My name is Jay Benedict and I’m a 66 year-old married man with children still in full-time education. I am self-employed, fit and active with no underlying heart conditions, nor do I have Marfan’s syndrome.
8 years ago I went to my doctor’s for a lingering chest complaint & the next thing I knew I was being sent to St George’s Hospital where I was diagnosed with sarcoidosis, a nasty incurable wheezing condition.
During all the standard tests, I had a routine x-ray, where they picked up what they thought was an enlarged heart: Was I an athlete? Was I in training? I wish! After more tests they managed to narrow it down to an enlarged aortic root. At 5.1cm, they felt it was nothing too serious and they’d simply monitor it for the time being.
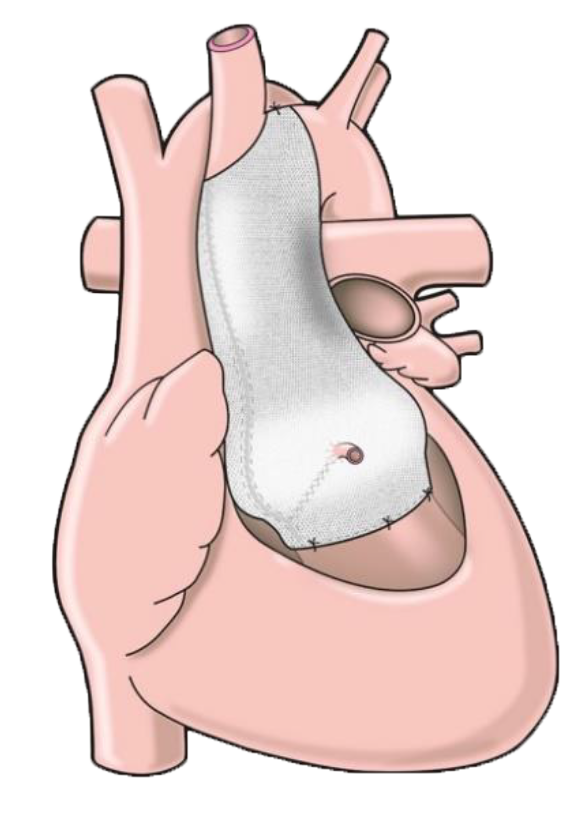
Professor Sutherland, now retired, told me that further down the line they might have to operate by wrapping a prophylactic around the aorta & sewing me back up. Fine, I said. The dimensions stayed the same for around 8 years. Then it started to creep up at the rate of 1mm a year. At 5.3cm with mild leakage in the aortic valve, they told me that my aorta was approaching the danger zone of 5.5 cm, at which point an operation would be inevitable.
So my cardiologist sent me to the cardio-thoracic surgeon at St George’s to see if I would be a candidate for valve-sparing aortic root repair. I found out that this operation was far more drastic than I had been led to believe: up to 8 hours on the table with good deal of that time clinically dead with the heart stopped by potassium, reliant on heart/lung bypass for life support, with the associated stroke risk that accompanies this procedure. Add in the body and brain cooled to approx 20º with the aorta cross-clamped, there was also a risk to the kidneys as their blood supply is via the aorta. If they couldn’t save my own valve, did I want a metal valve that would last a lifetime with the need for anticoagulants for the rest of my life or would I choose a pig’s valve that wouldn’t cause clotting but would need replacing every 10 years? This all sounded too invasive and I felt utterly deflated.
My wife spent the next couple of weeks looking for alternative ways to repair my aorta on the internet and stumbled on Tal’s brilliant TED talk where he spoke about PEARS: Operate on a beating heart? A 3-hour operation instead of 8? No lifetime of drugs? No chopping up & replacing the aorta? In fact no chopping at all – apart from accessing the chest cavity. I was under no illusion that sawing me open would be easy, but this was more like it. It was a no brainer.
Worried that a) I was too old for the surgery and b) it wasn’t available on the NHS, she wrote off one evening and received 2 replies first thing the next day; one from Tal allaying her fears on both counts and the other from Professor Treasure, who was no longer operating but recommending Mr Conal Austin at St Thomas’ Hospital, to whom he had already forwarded my wife’s email. She called me through to the computer to show me what she had found along with the good news I would qualify.
I asked my GP to refer me to Mr Austin for a second opinion. The next thing I remember was sitting in his office being offered the PEARS procedure. I couldn’t believe it really, it was like a miracle & so quick! I was about to become the 1st non-Marfan’s sufferer & the oldest by far ever to receive this procedure.
THE NIGHT BEFORE
Excited, nervous and trying to stay calm – what awaits me tomorrow? Thank God for the Temazepam for a good night’s sleep and my new pyjamas.
THE BIG DAY!
Outside theatre at 8.20am – thumbs up to Phoebe and the world’s still looking bright!
One hour out of surgery in Overnight Intensive Recovery – I haven’t woken up yet – high as a kite on Propofol and Fentanyl with a tube down my throat breathing for me.
It’s 1.00pm and they’ve started to wake me up but no one mentioned they have to withdraw that lovely cocktail of drugs as only the pain will bring me round – oh boy!
By 4.00pm, I’m fully awake and breathing for myself – blessed relief as they have removed the tube down my throat – oxygen mask only – sore throat like never before!
7.00pm and visiting time is over – a slightly uncoordinated effort at waving goodbye – having Phoebe there as I woke up was so reassuring and life-affirming! I was back in the room. And they say you remember nothing of your time in Overnight Intensive Recovery???
[I would say that the booklet they gave me said most patients remember nothing of their time in OIR. This is completely untrue as confirmed by all the other patients I spoke to on the ward. I was lucky because they woke me up during visiting time. I think my world would have been a lot darker without Phoebe’s voice as the first one I heard. When I squeezed her hand, the nurse told I’d squeeze anyone’s hand – it’s not true – I knew it was her. I even managed to say “I love you” to Phoebe in sign language! I also remember my surgeon, Conal, coming to see me and I asked him for a pint in sign language. Still they told me I wouldn’t remember. I did!]
DAY 1
Transferred to the High Dependency Unit – another patient described this point in the proceedings as feeling like you’ve been run over by a steam roller, that turned round, came back and flattened you all over again.
DAY 2
They’re determined I should sit in the chair as often as possible – coughing and deep breathing essential to clear the lungs – self-administered morphine on demand, thank God! Starting to resent the IV cannula in my neck though, that’s pulling sideways with the weight of all the lines they need to administer as few or many drugs as I may need. Gone briefly into AF (irregular heart beat that affects quite a large number) – they try beta blockers and then stronger drug therapy which eventually kicks in around midnight so no need for a jump start the next day.
DAY 3
After draining two tanks of gunk via a huge drain in my chest and they’re about to pull the tube out. Quick! Press down on the morphine clicker for the last time thank God – made me feel sick – paracetamol is working fine. Neck line is also removed – that’s a relief as it’s been tugging on my neck. Wish they’d remove the catheter as well, as I’m fed up with the commode. Although pleased to say the bowels are working fine – all without laxatives, as Phoebe insisted on prunes, apricots and figs from the moment I woke up.
DAY 4
Catheter out and a trip to a real loo – what joy. Back on the main ward as well! Portable ECG to monitor my heart beat and if they are happy with the trace over the next 24 hours I get to go home.
DAY 5
I do go home for Boxing Day – what joy!
Good food, tons of rest and sleep and daily walks are vital over the next few weeks. Learning to sleep on my back was the hardest adjustment, but sleeping at 45 degrees with a triangular pillow is a great help. I needed a bench seat for the bath and help to bath and get in and out of bed for around 10 days. It’s slow and steady progress but every day is better. Off the meds after 14 days as, with no underlying heart or circulatory problems my blood pressure was dropping so low I was dizzy much of the time.