In October 2018 I was on a business trip in Germany. Upon leaning forward to pick up my suitcase I experienced an unusual Ectopic/pvc sensation in my chest.
After having a very active life where the gym was the norm at least 3 x a week throughout my teens and until my late 20s and then various self-managed fitness regimes right up until October 2018, I was aware that the human heart can normally have such idiosyncrasies.
In the past I had always followed good practice and if anything had concerned me, I would speak with my GP and get it professionally dismissed.
Upon return to the U.K. I noticed this strange beat was unusually reproducible so after mentioning it to my wife she suggested I check it out just be safe.
In early December I went to see my GP who took my blood pressure, checked my oxygen levels and performed an ecg. I remember the technician performing the ecg saying, “Oh! that’s a bit strange but the doctor will check it.”
I returned home to work in my home office and a couple of hours later had a quick 4 mile run in my lunch time to try and get that healthy relaxed feeling. To be honest I felt well.
I didn’t think too much about my appointment until receiving a phone call that evening from my GP who sounded really concerned.
My wife was dressed up and ready to attend her Christmas work party when I received the call asking me if I was able to walk and if I was in pain. Surprised by this I answered no to both questions. I was then advised I should pack a case and get someone to bring me to hospital right away. I was in complete shock!
The hospital admitted me and placed cannulas in my arms. Doctors did many blood tests and I was attached to an ecg machine.
After several hours had passed, the cardiologist and nurse came to see me and said my T waves in leads V1 to V4 had all become inverted since my last ecg suggesting I could be having a heart attack! Thankfully, I wasn’t, and all my bloods, enzymes and troponin levels were completely normal.
I was discharged but with an advisory to follow this up.
I contacted my doctor and my healthcare provider the following week to get a referral to a cardiologist specialising in electrophysiology. I was able to choose who I saw, and I was lucky enough to be referred to Dr Riyaz Somani who was absolutely excellent and investigated me thoroughly.
After a plethora of tests including an event recorder, he concluded that the ectopics were benign and most likely stress or excitable tissue related but non-pathological either way and the inverted T waves implied a shape change in my heart. To be super-sure everything underlying was ok he decided a stress mri would be a good idea.
During this test it was discovered (but not yet known by me), that my aortic root and valve were dilated to 4.9cm and my ascending aorta to 5.1cm.
A couple of weeks later during a follow up appointment I was informed that my aorta was dilated, and this was gently introduced to me by Dr Somani. He explained it was an open procedure to fix this but that only monitoring was indicated at the moment and did I have questions?
I didn’t understand the full implications of this finding initially and had no knowledge of aneurysms other than they were a bad thing and that I would be referred to Leicester hospital for just routine imaging.
For a week or so I read various online support group posts to try and get my head around this topic, thinking I had maybe a 3.7 cm aorta or similar and that this posed little concern or risk.
Certain US hospital resources provided neat little tables regarding dilated aorta sizes and recommended lifting restrictions. I pitied those persons in the upper echelons of 4 cm not realising I was well in excess of that myself.
I was coming to terms with the diagnosis of the dilation, I thought “well it can’t be that dilated, I’m only being monitored” when I received the letter from Dr Somani to my GP with sizing information.
As soon as I saw this letter, and that my ascending aorta was dilated to 5.1cm, I crumpled into my chair and cried believing with absolute conviction that the life I enjoyed was now over.
For the next few days I tried everything to try and find some hope. I contacted the care team at my BUPA medical provider who supported me mentally and their cardiac care team started speaking with me.
I asked questions like was it a big job to repair this trying to compare it to coronary artery bypass surgery and was informed it was a significantly bigger operation.
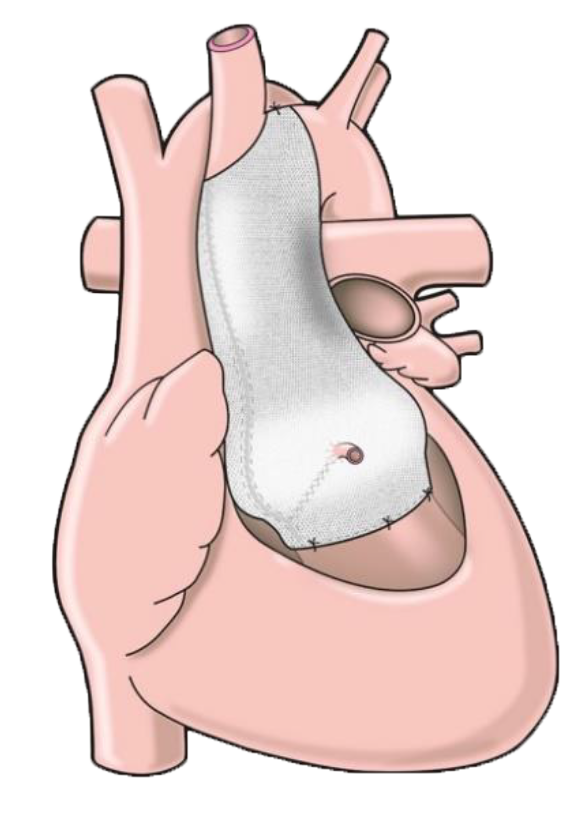
Whilst trying to get my head around a Root Replacement or similar procedure, I was fortunate enough to be contacted by a very helpful cardiac nurse named Takshila. She talked to me in depth about my situation and provided a lot of comfort. She said I may want to look into a new procedure called PEARS too.
A couple of months passed, I worked and researched my condition to try to get further acquainted with my options.
My research suggested PEARS was “the” best and safest option out there but particularly suitable for Marfan Syndrome sufferers who were largely asymptomatic and had a mostly functional aortic valve.
I knew I needed to find out if this was available for me with my standard non-Marfan anatomy and started my journey.
As part of my on-going monitoring and NHS care plan I had some meetings with a Professor at my local NHS aortic clinic and was provided some advice and options.
He wanted to try and get my aorta to last as long as possible and advised nothing is as good as what nature provides and so we should try medication to lower blood pressure (beta blocker) and use the measurement from CT and MRI scans to establish how quickly my aneurysm was growing or, in best case, find that it was stable. I agreed but was a bit shaken to be informed officially that as the aneurysm was over 5cm there was a risk of rupture.
I continued to try and educate myself on all matters of the aorta to try and establish what I wanted and what may be best for me when the time came.
At this point some friends commented I was maybe jumping the gun a bit but I always found detailed planning to be a good thing.
I read every internet document I could lay my hands on regarding aortic aneurysms, the treatment options, mortality rates, numbers done at each centre of excellence around the world and results of every study I could find.
I watched every talk, online Cardio-Thoracic surgery discussion I could and tried to find every development that could apply to me.
The months rolled by and my new un-fitter, fatter, depressed self, emerged much to my dismay. Any person who has been in this darkest of places prepared by such a diagnosis and faced with the prospect of imminent death every day can relate, I’m sure.
I went for my 6 monthly scan and lo and behold my aneurysm had grown another 1mm. The NHS professor’s concern was clear, he said with that growth rate we need to sort you as soon as possible and reassured me that the CCU was ready if I should need it. He also advised it would not be long before the aneurysm started pulling my aortic valve apart making regurgitation a problem. He kindly checked this for me.
At my second appointment he said I needed to give some thought to how I wanted this to be fixed, I went away finished my comparisons and presented a short summary to get the objections/advice at my next meeting a few weeks later.
After many more hours of research, my Choice #1 was PEARS.
My reasons:
- It burns no bridges
- Own endothelium is retained.
- I likened the concept to placing a weak balloon in a net bag. Much stronger than stitching a tough patch on the balloon.
- Operations usually done on beating heart and in a few hours.
- Heart attack and stroke risk minimised as operation was not so long and bypass usually wasn’t needed.
- No re operations seen so far.
- Utilising rapid prototyping and 3D printing to prepare each personalised device.
- Only 1 patient lost due to the operation.
- The surgery was much less intense than other options for the patient.
This was a no brainer.
My #2 choice was Valve Sparing Root Replacement. This I kept reading is the “Gold Standard” and would be the preferred standard way to fix my problem.
An appointment was fixed with a surgeon who had vast experience of root replacements, so wanting to be completely open minded I accepted as I thought it may also be my only choice if medical constraints unknown to me (as a non-medical professional) dictated this and I needed to know the full picture from all sides. My medical insurer, BUPA, advised I do this too.
Just like the other Professor, he was a very nice man and a highly regarded surgeon and spent a lot of time explaining root replacement surgery to me.
I took it all in and also wanted to hear his opinion on the PEARS device option.
The NHS guys were very passionate about their solution and said I should not ignore the amount of these successful operations worldwide. They worried that PEARS devices were a bit new, they worried they could move, trapping a coronary artery and had concerns about that the longevity of PEARS devices was still not really known. Finally, they said we know that it is great for Marfan patients but that I am not Marfans.
I carefully noted these objections/concerns.
It was then I thought back to an inspiring TEDx talk and watched the story of Mr Tal Golesworthy. I wondered if he could help me clarify if PEARS could still be an option for me as a non-Marfan patient or if I should forget it due to my standard anatomy and the concerns raised for me as an individual.
I sent a Facebook messenger message to Tal explaining my situation, half-thinking there is no way this pioneering hero was going to respond to a request from me.
To my absolute amazement and delight Tal messaged me back answering every question I had incredibly comprehensively and with great clarity adding more compelling reasons to those I already knew. He not only put my mind at rest about the concerns raised but pointed me at clinical evidence that clearly showed why the concerns were not valid and why I would most likely be suitable.
Additionally, he said I could call him if I wanted to talk.
There were still many hurdles though. Would I still be suitable for PEARS after being checked by their surgeon? Also was the treatment available for me on the NHS or via my private medical insurance?
I started trying to find out.
It was clear the NHS surgeons felt comfier with a valve sparing root replacement. I firmly believe that this is because it’s what they know best and know what they can deliver. However, in conversations, all of them advised that keeping one’s endothelium is better than any man-made option that is available, also that cardiac mobility is reduced with a traditional aortic graft and re operation at maybe 60 years of age is quite normal.
At the same time with PEARS I was intrigued reading about no re-operations, no cardiac mobility issues and I read about an earlier patient who had passed away from an unrelated cause and that when his aorta was checked it was found that within the graft the histology of the aorta was again normal. It had been able to repair itself!! (hope ?)
As no one could really say when a person’s aorta will rupture exactly (only that the risk sky rockets around 6cm), and actually felt healthy, I really wanted to try and keep my own parts and give my natural body parts some help rather than cut them away.
I spoke to my private medical provider (now Healix, changed due to a company decision) to check if they would cover me for PEARS. To my horror they said no and that PEARS was regarded as experimental. I was gutted but mentioned that the previous provider had recommended it and advised it should be covered.
In fairness Healix contacted me back quickly and said it would be rather unfair if they did not cover this if BUPA had agreed to. Also, they said they would only do this if there was irrefutable proof it was best for me as the patient.
Numerous investigations were done and I provided my evidence to my nurse case manager Nicola Fee who I felt genuinely wanted the best for me. I felt the evidence provided was compelling and Healix did their own research.
Towards the end of 2019 I had my appointment with the Cardiothoracic surgeon to discuss a valve sparing root replacement.
Nicola contacted me shortly before and said we would like to provide you a second opinion and an opportunity to talk with Mr Conal Austin. I was absolutely delighted but also tried to be open minded as it looked like PEARS due to one reason or another may not be available for me.
One week after meeting with the valve sparing root replacement surgeon I met with Mr Conal Austin. Amongst many other accolades I was aware that Mr Austin happens to be the world-leading specialist PEARS surgeon. He reviewed my case and I was delighted when he confirmed every hope I had about the procedure and its expected results. We shared the opinion that PEARS was my best option. I relayed this back to my Healix nurse case manager and crossed by fingers.
It was now heading towards Christmas and sleepless nights were common. I was trying to keep a brave face but was consumed regularly worrying about my aorta, would I be able to have a PEARS device, how long was my aorta going to last, or, if not, was I strong enough to get through the planned massive standard surgery?
Just before Christmas, Nicola from Healix contacted me to advise they would pay for my PEARS surgery. I was delighted as was she and another colleague Nicola Brundrette who had also helped me from the BASF side.
I won’t ever forget that evening. Having tried to limit discussions I soon realised the massive relief my wife and 2 children felt from this decision, it was quite a moment for us all.
For the next step just before Christmas my wife Kate and I were travelling down to London Bridge hospital for my PEARS CT scan. This is where a special 3D scan of my aorta would be made and from that a former for my PEARS prosthesis could be made.
The scan went well and just after Christmas I was advised of a target operation date of 24th January.
Mr Austin’s PA, Mrs May, kept me informed at every step of the way and Tal regularly contacted me offering advice and support (what a human being you are, sir!)
As the 24th approached I was contacted, all was on schedule and my wife and I travelled to London Bridge hospital for my pre-op assessment.
My pre-op assessment was carried out by Mrs Suzanne O’Connor a cardiac sister at the London Bridge hospital. She was extremely patient, calm and thorough. She took me through exactly what would happen on admission and explained that other than a couple of cannulae being inserted into my hands/wrists all other lines, catheters and tubes would be placed whilst I was asleep and under general anaesthetic.
This was very re-assuring. She also explained detailed answers to every question I asked regarding my planned time in hospital and recovery.
My wife and I returned home, I felt surprisingly relaxed and positive. It was happening, these people were so professional and I really believed that they were going to “hopefully” save my life.
On Thursday 23rd of January, my wife, Mum-in-law (to kindly support my wife) and I all travelled down to London to ensure I made my surgical appointment.
I had expressed to Mrs May (Mr Austin’s PA), that I was keen to share my story as I wanted to help others in a similar position to myself. A very nice lady named Sam Boyce contacted me and informed me they could give me the opportunity to tell my story in a short film. It was a bit out of my comfort zone to do such a thing and being no Tom Hardy I was a bit daunted but grateful that I could maybe help someone else in my position.
Sam and her camera man Ross met me in my hotel and without any pressure or inconvenience let me tell my story.
On Friday 24th 8 a.m. after a rather patchy night’s sleep we travelled to London Bridge Hospital.
When we arrived, we were politely greeted by a concierge and then a porter who took us to my room and explained room facilities to me. These were all steps accurately described by Mrs O’Connor.
Once there I met my first assigned Cardiac Nurse Vick Gonallason (hope I spelled your name correctly?).
Vicky started taking great care of me from me the moment I arrived and helped me prepare for the operation.
For the next few hours I was visited by a number of persons one by one. The ward doctor, the anaesthetist, the cardiac sister, nurse in charge and finally by the surgeon Mr Austin.
I was very taken by how incredibly professional and personable every one of the hospital personnel were. You often hear in life, “oh you are in good hands.” I’m often a bit sceptical with that, but in this case it really was a statement of truth.
During all the anxious times one thing I want to point out is that Mr Tal Golesworthy was in regular contact with me, he was able to relate to each stage as I approached it and totally out of the goodness of his heart was mentoring me at every step.
Finally, the time came where Mr Austin briefed me about the final plan, I was given my sedative and taken down to the theatre.
As I went into the lift, I kissed my wife goodbye, the love in her teary eyes and shaking hand made me choke back tears as I hoped so deeply to see her and my daughters again.
I was welcomed into the operating theatre prep room where my nurse, Mr Rayner (chief perfusionist), anaesthetist (Dev) and the other team members welcomed me. I remember them saying, “don’t worry James we’ve got you.”
The next thing I remember was waking up with a heavy chest and tight feeling lungs but seeing my wife’s face. My first words were “Have I made it?” She simply replied, “Yes babe!” I then fell asleep again and apparently woke up a further 5 times declaring I had made it with a fist bump added for good measure. Kate did say by the 5th time it was starting to get a bit old ? ?
The intensive care period seemed to pass quickly. The pain relief was very effective and the on-tap drug (Fentanyl, I think), administered via a self-regulated green button was a godsend.
Despite having a slight wobble when my chest drain was removed and going sweaty and hot, an excellent doctor called Thanos kept me calm and gave me brilliant care. There were others too, but he was the poor guy I focused (unintentionally) my worry induced requests on. Thank you Thanos for putting up with me, you were amazing ?
Saturday 25 January
I was taken from intensive care back to my room. I was cleverly manoeuvred from one bed to another.
Upon getting into bed the pain was better controlled than I had imagined it would be but my lungs still felt the size of peanuts. Oxygen was provided but every breath for the next 24 hours felt earned.
That night seemed to last for ever. When morning finally came, what felt like a week later, a stream of medical professionals began their work. Firstly, I was administered more pain relief, all manner of tests were done and finally the nurse in charge came in and informed me they would be getting me out of bed in the next hour. I was quite surprised and thought there was no way I was going to be able to do that and in my head I thought, “Good luck with that.” ?
To my amazement one hour later I was showered and sitting in a hospital chair ready to meet my wife at the start of visiting hours. I’m not going to lie, I felt like I had done 10 rounds with King Kong but I was quite amazed I was able to sit up, function and enjoy the company of my wife. I still was rather sleepy and had a few naps but fortunately my Mum-in-law was there to keep my wife company.
Later that day when the physio visited, I even managed a few easy stretches and took my first few steps. I went to bed that evening quite surprised by the degree of progress.
Sunday 26 January
I had quite broken sleep and some discomfort on the second night in my room. But the nurses were there seconds after my call button was used, to see how they could help. Pain relief was administered, I was checked and about 5 hours sleep was managed.
Upon waking in the morning, pain relief, the by now usual tests, and breakfast was delivered. I had little appetite despite the food being amazing but noticed an improvement from the day before. It seemed quite small, but it was there. By the time the second evening in the ward had concluded I had completed the orchestrated daily plan of recovery. My wife commented that I seemed a lot better. The medical team at London Bridge had again worked magic, I noted my progress too and the team had me walking, in less pain and were managing any symptoms I had very effectively. I thought, “Wow these guys are incredible.”
Tal texted me to check how I was feeling. He followed up with a call when I said “a bit better” and explained how my recovery would probably be non-linear with ups and downs but with overall gradual progression. I have to say his description was brilliantly accurate and helped me a lot.
Monday 27 January
I managed a bit more sleep on Sunday night and although there were a couple of waking hours, there was more sleep.
I noticed getting up and going to the toilet in the night was getting easier.
On Monday I was able to shower, dress and have my breakfast independently. After the medical team and nurses had set my daily goals and scheduled my tests my wife turned up and I again mentioned how much better I was looking.
Despite all the progress and so as not to mislead anyone, I should point out there were still some expected lower points and effects of the procedure that I was dealing with during the whole time. The weaker feeling breathing, a temperature that would occur once the pain relief was wearing off and some minor visual disturbances.
Tal called me to check again how I was and explained every symptom I mentioned in detail. It was a great comfort especially as each gradually passed as he advised they would.
The nurses during this time additionally made me feel very confident with explanations of various symptoms too, the treatment of them with medication and then this all checked and overviewed in the evening when Mr Austin arrived. He was extremely re-assuring and provided answers to all my questions and provided details of the excellent repair he had done.
Tuesday 28 January
Another slightly better night’s sleep. By the time my wife arrived I was showered, dressed, breakfast eaten, and I felt a bit more like my usual self.
I did notice a slightly quicker heart rate since waking up and fairly frequent ectopics but I noticed both these start to reduce as my lungs improved and my oxygen levels began to normalise. As the day passed and I completed various tasks I again noticed I was improving.
One of my daily appointments was getting an echocardiogram to see how my aortic valve was functioning. In previous NHS appointments I was informed that my valve had a degree of regurgitation, although it wasn’t giving me problems yet I was advised that as the Aneurysm pulled the valve apart I should expect it to start to fail and experience symptoms.
Much to my delight the PEARS device was now securing my valve in place and the cardiologist performing the echo told me no regurgitation was visible now. Great not only was my aorta fixed, so was my aortic valve ?
I steadily walked back to my room a happy man.
The Cardiac sister came to see me in the evening and asked a lot of questions and provided a lot of about how I felt I was doing, as did Mr Austin. Both mentioned discharging me on the coming Thursday.
Wednesday 29 January
More nurse, doctor and physio visits followed. I was aware I was experiencing some rehabilitation excellence.
By now all cannulae and all wound dressings except the stitch and plaster covering my chest drain wound were removed.
The frequent temperatures were becoming less severe and I was reminded about the many provided techniques to work on my mobility and lung function.
I was by now doing steady hourly laps of the cardiac ward with my wife and feeling slightly stronger every day.
Thursday 30 January
Discharge day ?
My morning routine went well. Showered, dressed and breakfast eaten all a smidge easier than the day before.
My travel back home was arranged, and I received the message that my brother in law, was on his way to collect us.
Final medical checks were done, the pharmacist came to my room to thoroughly explain my medication schedule and to provide the medication.
Sister O’Connor came to my room and went thoroughly through what the next week of my rehab should look like. After carefully explaining all the support framework available to me, my mum and brother-in-law arrived to collect my wife and me.
The absolute delight on my Mum’s face to see me alive and well made me slightly emotional. Sister O’Connor spent some more time with us all explaining all support aspects until it was discharge time.
I tried to say goodbye and thank you to all of the people who had looked after me so well. A couple were busy and off shift but I am sure I will get the opportunity to say thank you on my follow up visits.
So, I left the hospital, surprisingly quicker and in better health than I had imagined.
The car journey home despite my brother in law’s kind efforts to plan a nice interesting and entertaining route had a fair number of traffic humps and potholes which where an “interesting” experience which my heart, shoulder area and back didn’t like too much.
About 4 hours later after a mid-point coffee stop we arrived home.
The first night in a bed was challenging as expected but with the help of a pillow my wife got for me and some thoughtful pillow arrangement a good night’s sleep was possible.
Now I am at 2 weeks post op. I am following my rehab directions closely and have been doing everything I have been told to by the medical team at London Bridge Hospital. Every day I feel some progress and feel more and more hopeful that my fully fit self is something I can look forward to again in the not too distant future, in fact, I feel it coming closer every day.
I will remain eternally grateful for the fantastic job Mr Conal Austin, Tal and all the team at London Bridge have done for me. They and all the people involved in making this happen for me have given me a future to look forward to with my family and my health. I really cannot think of any greater gift one could be given.