I am now 34 years old and I have Marfan syndrome. I am also a GP in England. I’d always been told I had a ‘mild’ form. I decided to undergo IVF with pre genetic disease testing and in July 2019 I delivered my healthy marfan-free baby. My heart scans had been fine throughout but then on a final routine monitoring scan it was found that my aorta had gone from 41mm to 48mm within 3-4 months. I was devastated. However I knew I wanted PEARS from the reading I had done and I got in contact with Mr Austin’s secretary who very happily saw me urgently. He agreed I needed surgery and was the perfect candidate! He did say he would have operated pre-emptively prior to pregnancy. This was frustrating as my cardiologist had refused to refer me when I had asked a few years prior.
It did not take long to organise the CT scans required, which were organised locally for me to save travelling (I live in Sheffield, not London!). Unfortunately it was delayed due to COVID but then I got my date in July.
I travelled down the day before the surgery and got settled into the bay. Below is my day by day relocation while in.
Day 1
My surgery was in the afternoon, however the nursing staff get you ready in the morning in case they take you in early. I had the frustration of being told I was going down at 11 but didn’t until 2pm!
When I was in the anesthesia room it was a very jovial atmosphere. I was given a sedative and can’t remember much else. They put multiple lines in you while asleep, so you don’t remember these going in which is great!
My husband tells me he got contacted around 5pm by Mr Austin to say I was okay. The first thing I remember was vaguely seeing several heads looking down at me and then the next thing it was 7pm. I don’t remember the ventilator being removed, but that was done in theatre.
Unfortunately I had a bad reaction to the anesthesia and I woke to find myself horrendously nauseous and vomiting and had several anti sickness medications with limited effect. The staff were great and very supportive throughout this.
I had a pain button at first to help as well, which was great, but they had to keep making me press it as with the sickness I was reluctant. I understand my level of sickness is very rare!
Day 2
I still felt very sick but was no longer vomiting. The staff were very happy with me and I moved from ITU to HDU that afternoon. Most of the day varied between drug induced sleep, awake and feeling sick! The day went in quite a haze. Apparently I kept sending jumbled texts to my husband!
Day 3
Finally on top of my nausea, I managed to eat and feel a lot better for it. Still had a lot of drug induced sleep but felt better in myself.
All of my lines came out today – chest drain was uncomfortable but only for a second and I felt like a new woman when it was removed!
Removal of the arterial line in my wrist and Central line in my neck didn’t hurt at all. It made moving immediately so much easier and I felt much more confident about sitting up. I also changed my pain button to oral medications only at this point – which was a joint choice between me and the doctors. I am pleased I dropped down as it cleared my head. I think most people’s lines are removed a day earlier but because of my sickness they kept things for longer.
Once everything came out I was moved to the ward an hour later – I walked independently too, which felt great.
Day 4
Finally no sickness and started to stop the sickness tablets. I did struggle with pain more but that was because of moving about more. If you ask the amazing nursing team they will bring pain meds. It’s important to have your pain controlled enough so you can cough and take deep breaths. Holding a rolled up towel against your breastbone will be your best friend!
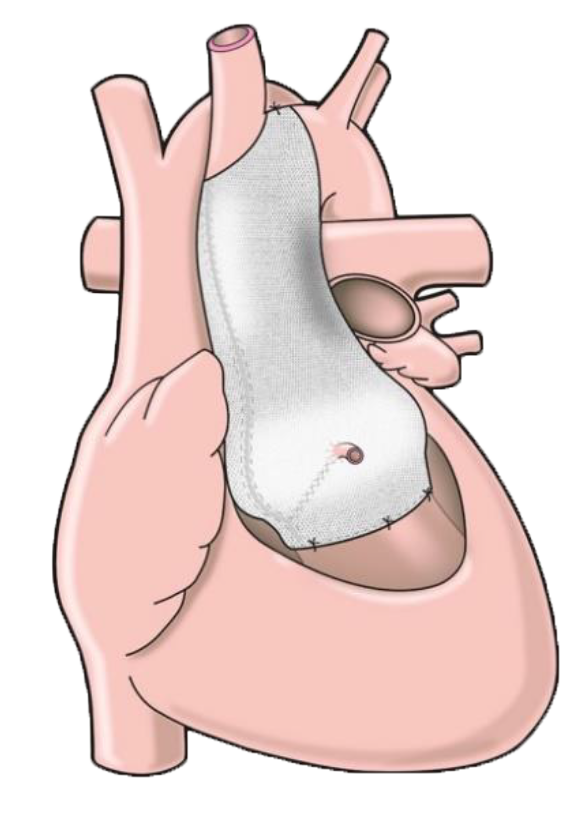
Sadly I spiked a temperature this afternoon – 38.6 and it stayed there for a good 12 hours. Otherwise I felt better. Some extra tests were done but this was due to an inflammatory reaction to the PEARS rather than any infection.
This night was the first night I suddenly didn’t feel unwell and poorly. That feeling left. I was still in some pain but I no longer felt unwell. This was the turning point for me.
Day 5
I had a chest X ray and echo and was kept in to make sure my temperature stayed down. (Which it did.)
Also my transport needed 24 hours to organise as I had to travel from London to Sheffield via hospital transport due to shielding post surgery from COVID.
Day 6
Home! I was nervous about the journey but actually it wasn’t too bad. I got home and went to bed.
Day 7
I felt really poorly today. I think the travelling had exhausted me and my body was telling me I needed rest. It was a hard day. However, I quickly improved.
Week 2
I kept things steady but felt a lot better being at home and quickly weaned off my pain killers. I was still resting and sleeping a lot.
Week 3
I felt a lot better and started doing 20 min flat slow walks around my garden. It was only the discomfort from the sternum which was slowing me down.
Week 4-6
A bit of a blur but more of the same – more walking, more feeling like normal and getting my energy back. It came a lot better than I thought it would. Biggest issue was doing too much or knocking the sternum – which happened a lot with managing my 1 year old at this time. I managed to have guests and friends around to see me which was great.
17 weeks post op
I was back to work as normal and back to doing all things outside that I love. I could carry my 1 year old on my back and go walking in the peak district with little to no problems.
1 year post op
No problems, back to normal.
Occasional niggles from my sternal wires but that is it. I am back to living my life as normal. The scar has massively improved and it’s much fainter in appearance.
Now
I am now 3 years post op. I have had no complications or issues and all my follow up scans have been fine. My aorta now measures around 45mm on my annual MRI follow up scans. I run, hike, climb, carry my now preschooler all without any issues. I very rarely get some sternal irritation and that’s it. The only reminder is my faded scar which looks better every year.
My advice if I had to go back in time – advocate for yourself. If you want this procedure don’t wait until it’s too late – push your cardiologist for a referral to someone who does PEARS.
Advice if going for it
- Bring comfortable PJs which are easy to get on and off.
- I find listening to audiobooks great and relaxing the first few days – particularly when i didn’t want to read/feel up for it
- Ear plugs can be useful for sleeping at night time and a mask – wards are busy.
- It feels impossible but sitting up and moving about as soon as you can helps with recovery.
- Accept a rolled towel to hold against your chest when walking and using the toilet. It makes the pain better.
- Don’t get constipated!