I had my PEARS surgery in mid November 2020 with Mr Petrou at the Royal Brompton in west London. This was of course in the midst of the Covid-19 pandemic. In this testimonial I have focussed on the run up to and recovery from the surgery, as other people have already covered the stay in hospital in some detail, and my experience was similar to theirs.
I had for many years been aware that I have Marfan syndrome due to my family history, I have been aware for about a decade that I would one day need surgery on my aortic root, and had been monitored in the Liverpool Broadgreen Hospital under the care of Mr Oo and Mr Kudevali, I’m now in my mid 30s. The aortic root had slowly increased in size over a period of about a decade until it tipped over the 4.5cm mark, and when it got to around 4.6cm I was advised to get on with investigating and deciding on the surgical route. Due to other life distractions, and my natural inclination to put this off, there was a bit of a delay until I started investigating surgical options in earnest.
Mr Kudevali had outlined the options, my next step was to call up the Marfan Trust where I spoke to Dr Anne Child. I believe Dr Child to be hugely knowledgeable on all things Marfan related, and for anyone considering aortic surgery options, or other Marfan related life decisions I would strongly recommend picking up the phone to her, via the Marfan Trust website.
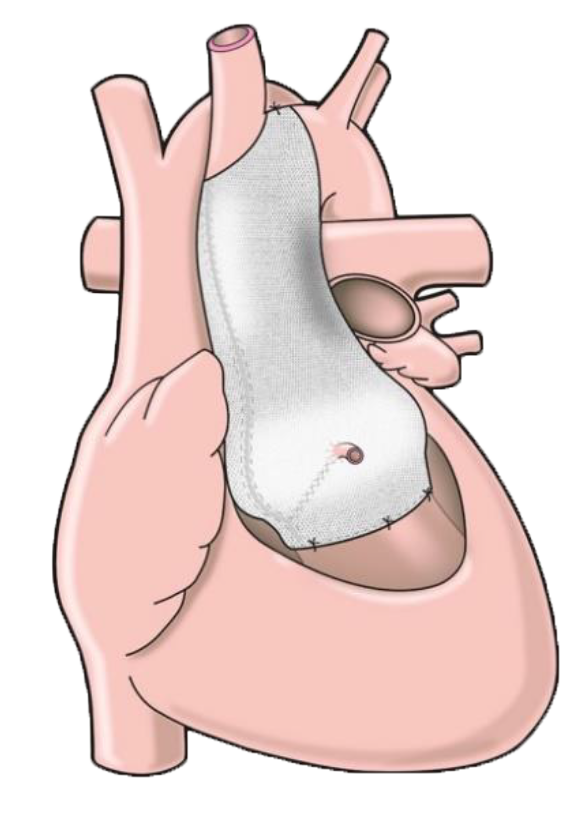
Dr Child discussed with me the options of PEARS (Exstent) route, and the root replacement option with or without sparing the heart valve. From this conversation and other research I had done my mind was pretty much made up that the PEARS route was the one for me, the cold facts as I understand them are that the recovery time for PEARS is likely to be shorter due to it being somewhat less invasive, and that PEARS doesn’t necessitate lifelong warfarin, unlike the Total Root Replacement option. Added to this the engineering thinking behind this procedure appealed to me as an architect. The relative ‘newness’ of the procedure didn’t put me off, for me it was about weighing the options based on their merits, rather than on how long each option has been in existence. Dr Child pointed me towards Mr Petrou, partly because of his experience in performing both the PEARS and the root placement procedures.
Dr Child wrote to Mr Petrou on my behalf, and I was then contacted by the Brompton for a consultation with him, which was over the phone, Mr Petrou then spent some time going through various options. One of the points about Mr Petrou is that he has a lot of experience in performing both the PEARS procedure and the root replacement options, and this fact helped me to be able to trust that he was giving me a measured view of both options. After this I felt quite reassured that the PEARS procedure was the right option for me. With Mr Petrou there was also the factor that in the unlikely event that the PEARS turned out not to be possible during the surgery, then he could instead perform the root replacement procedure.
The timeframe for having the operation was around 4.5 months from the conversation with Mr Petrou. Obviously the NHS is and was dealing with a huge amount of pressure in late 2020 related to Covid-19, and there was a degree of uncertainty about the surgery date, I had asked for a month’s notice for the surgery if possible. This for me was the most stressful period, owing to being in full time work and with caring responsibilities, all in the midst of the pandemic, and not knowing if I might have to drop everything at short notice to go off for surgery, or that it might still be several months down the line, which made it very difficult to plan anything. In the end I was able to have a month’s lead into the surgery, although this did mean it was 2 weeks later than it could have been. In retrospect given the national situation it would have been wiser to take the first possible option, hindsight is always crystal clear! I was fortunate that the surgery went ahead on the date as planned.
I was also worried about the procedure itself, as I imagine most people would be. I eventually found that the best way to think about it was that really it was all in the surgical team’s hands, they’re experts at it and they do it every day, just as I do my job every day, and actually it wasn’t really my problem to think about any issues that might come up, as after all I’ll be unconscious at the time! All I could really do was make sure I was in good shape, be careful about Covid and turn up on the right day.
There were some challenges in getting to hospital and back, and to the pre-appointment in the most Covid secure way that I could. There were 2 separate Covid tests in the run up to the surgery, and there were no visitors allowed, and this meant my surgical route was described by the hospital as a ‘Covid secure pathway’. From the perspective of someone who hadn’t left the borough where I live on the other side of London for about 9 months, it was quite mind blowing to go across town and into hospital, seeing the London sights along the way!
I’m not usually a fitness nut, but in the run up to the operation I had decided to get a bit fitter, and I’d set up a fundraising page with the aim of doing some jogging twice a week and yoga every day. I’m really glad I did this, it really helped to calm me down, give me focus, and give me a degree of control over the situation. It was also quite a good way of explaining what I was going through to people & colleagues. I therefore felt very smug when, having checked into hospital on the Sunday, the nurse taking my blood pressure said ‘I just need to ask, are you an athlete? Your pulse rate is very low’. I was pleased that the running and stretching had paid off, and told a lot of people this story, but I also feel that being a bit fitter helped my preparation and recovery and possibly made some of the decisions around medication and recovery afterwards a little simpler.
Various pre-operation tests including a further Covid swab were done between the Sunday and Tuesday, and I started to adjust to hospital life, which was quite an adjustment from my lockdown routine at home, and also felt fairly happy that the Covid risk was as low as possible. In this time Mr Petrou came and visited to run through things, as did various other doctors and nurses, including the anaesthetist, and there was the obligatory paperwork to sign, including giving permission for the team to opt for the root replacement operation in the unlikely event that the PEARS procedure turned out not to be possible.
I had brought a couple of easy going books, and downloaded a few audiobooks, podcasts and music, which was helpful in passing this time, and taking my mind off things.
Having fasted from the Monday night, time dragged by on Tuesday morning with my stomach rumbling, and of course phone calls to my family. I was then wheeled away to the operating theatre, and the last thing I remember was saying, ‘I feel a bit nervous’, I’m pretty sure the anaesthetist used this as his cue to knock me out – probably the right decision! They only put in the wrist cannula before the anaesthetic is administered, the various other lines go in after this, which is a relief as like many people I’m not keen on needles.
The next thing I remember is waking up, and being told the operation was complete and successful, everything was very bright and I had a breathing tube in, so couldn’t speak. My memory is a little hazy about exactly what happened when, and other people’s testimonials have covered this in some detail, so I’m not going to focus on this in too much. I do recall everything being very bright, and my eyesight being worse than usual for the first couple of days, but this gradually returned to normal. I also remember feeling pleased with myself for finishing off my breakfast the next morning, then promptly throwing up in the direction of the ward round doctors, I think they forgave me. The general procedure is moving from post operation recovery, then being moved to High Dependency (HDU) then to the ward. At each stage a few more wires are pulled out, and the reliance on pain relief reduces, at first through a self administered clicker, and then via pills and oramorph (oral morphine).
I had packed quite a lot of things like snacks and changes of clothes, but in fact didn’t really use much of this. The hospital gives a list of things needed such as dressing gown, pyjamas and slippers, and I actually don’t think I needed much beyond this list. The main thing I found that I wasn’t really prepared for was the mental wellbeing aspect of the recovery, in particular the cumulative effect of the medication having an impact on my mental state. Once I was back on the ward I found that I started having very unpleasant and lucid dreams, meaning on some nights I couldn’t really get much sleep, and this affected how I then felt in the day. One element of this was that I was given losartan just before bed. Only after the lucid nightmares I recalled that this was the reason why I would normally take losartan in the morning, and never before bed. I found that it was helpful to have some classical music and relaxing audiobooks to listen to to pass some of the night. I don’t think everyone has this side effect but it’s good to be prepared.
On the ward I had most of the remaining drips taken out, but the last one was the central line (in the neck) this one really started to get on my nerves as it was hard to keep my head and neck in a normal posture without the line painfully moving around and flopping over my shoulder, so I ended up leaning my head over to one side most of the time. After I asked if there was anything that could be done, the nurses were able to tape it up to my jaw area, which although I looked a little more ridiculous than I already did, this did help reduce the pain quite a lot. In retrospect my bad posture probably contributed to me having lots of neck pain over the next month or so of my recovery, so I wish I’d asked them to tape this up earlier.
Overall I made quite quick progress, and I was able to leave on day 4. I’m not a very patient person, and although the care had been amazing, I really couldn’t wait to leave, and to eat a home cooked meal. With the Covid situation there were some logistics to think about. There seemed to be some unwritten rules about who was eligible to get hospital transport and who wasn’t, I seemed to be firmly in the category of those who weren’t eligible. In the end I got a black cab from outside the hospital (these come by regularly). Although my time in hospital was positive and I have no complaints, quite the opposite in fact, it was a massive relief to escape and finally get home and return to my family and to eat home cooked food.
A few days after I was home I woke up in the morning with a rapid and irregular heart beat, I knew that aortic fibrillation (AF) to be a fairly common side effect post surgery, but it does feel very odd when it happens. Due to Covid I was nervous about going straight to my local A&E, but in retrospect this is definitely what I should have done. My route to the local hospital was via the GP who did an ECG, and then by ambulance straight to hospital where I ended up in re-sus, this was fairly stressful, although perhaps not quite as dramatic as it may sound. They were able to give me amiodarone to regularise the pulse, and this got things sorted out quite quickly. I was very keen to get home before my birthday, but I ended up staying in for a couple of nights. The highlight of this visit was when the two night shift nurses woke me up bright and early in the morning by singing happy birthday at the foot of the bed, and telling me I was going to be discharged that morning!
After this I was put on a low level of beta blockers, when I later discussed it with the doctor back at the Brompton they did say that they would normally prescribe this post surgery, so I’m not sure why I wasn’t on it in the first place, perhaps there are differing medical opinions on this.
When I was home, there were a few practical things I found helpful, firstly having an anti-slip mat in the shower, as I did feel a bit unstable for the first few weeks. Also having a few big pillows to help me to sleep at a slightly elevated angle for the first few days. Quite quickly the pain of the operation started to subside, and I was able to cut out the painkillers after a week or so, this was fairly quickly overtaken by neck and back pain. In particular when I started to go for longer walks my neck and shoulders would get increasingly painful after about an hour, this being the winter the thing that helped this was dressing up really warm, with a couple more layers than I would normally wear. Also I was given a snood to keep my neck warm, which I started wearing pretty much all of the time as this seemed to really help. I was continually hungry for the first month or so, and the advice is to get lots of calories, so it was nice to enjoy some guilt free treats.
At around 8 weeks post operation I’ve been able to start doing quite long walks for several hours, and to do a short, light fitness and stretching routine, obviously without putting weight on my arms. I have felt quite a lot of fatigue, and I’ve needed fairly regular naps, although this has reduced a lot by the 8 week point. I expect it will be around 3 months until I feel ready to go back to work, on a part-time basis.
I hope this has been helpful to those considering and planning for having the PEARS procedure. I’m sure everyone’s experience is different, but hopefully some of these points are useful to others in preparing for and recovering from the surgery, I would just end by saying that although at the time the surgery and the run up to it was very stressful and a real ordeal, it is a huge relief to have this behind me, and not have to worry any more about this issue, and be able to now look forwards in my life, so a huge thanks to Tal, and the team at the Brompton for making this possible!