I was diagnosed with Marfan Syndrome as a teenager following an excessive growth spurt. I have classical musculoskeletal features and a dilated aortic root and mitral valve prolapse. I lived a sensible life and my heart was being monitored by regular Echocardiograms so I wasn’t unduly concerned until my sister died suddenly of an aortic dissection in 2018; she was 52. An MRI scan was actioned and my aortic root measured 46mm. A year later it measured 47mm and I started to worry.
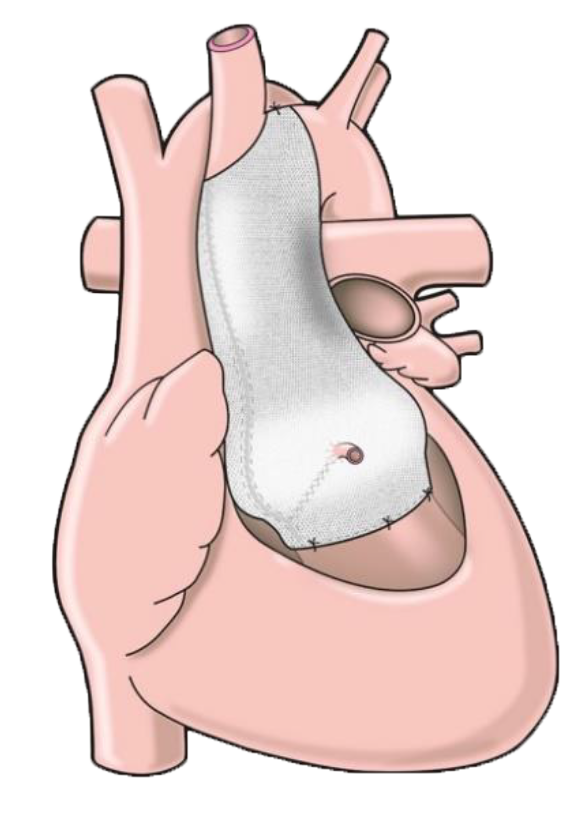
I began researching surgical intervention for Marfan patients and came across the PEARS procedure. The more I read about this and studied the medical papers, the more it made sense. So I wrote to a leading surgeon, Mr Conal Austin, to seek his advice and before I knew it I had an appointment to see him. Having Marfan Syndrome and with a family history of aortic dissection I was a suitable candidate for PEARS and the ball was set in motion.
I have never had an operation before and, being particularly needle phobic, fear and anxiety set in. In addition I have M.E. (Myalgic Encephalomyetis) / Chronic Fatigue Syndrome with an acute onset following a virus when I was 35, which challenged me further.
Despite the daunting journey ahead of me, the internationally renowned Cardiac Team at Guy’s and St Thomas’ was excellent, helping me through each twist and turn of the journey. Upon first meeting the lovely surgeon, Mr Conal Austin, his personable nature put me straight at ease. Having extensively researched the PEARS procedure, I was confident in the operation, knowing too that Mr Austin was the best in the world, having carried out well over 100 operations of this type – so the operation itself was not of concern as I was in the best possible hands. Mr Austin also put me in touch with Tal Golesworthy, the inventor and first Marfan patient to have had the personalised ExoVasc fitted in May 2004. Tal was an equally approachable man and was able to allay some of my worries, being openly available via e-mail or at the end of the phone. Specialist Congenital Heart Disease Nurse, Alex Corless, helped me through my needle phobia by introducing me to Emla cream (an anaesthetic cream that numbs the area beforehand) – which was applied before all blood tests and cannulation. Alex also talked me through the whole operation and what to expect at each stage. I also benefitted from the support of my cousin, a Doctor at Guy’s and St Thomas’ and, whilst cardiology is not her field (she is Clinical Lead of Nuclear Medicine), she knew the hospital and medical procedures well. With all the right support in place I felt more comfortable about the upcoming operation.
When I was first told that my personalised ExoVasc had been made and I was offered an operation date, I went into panic mode. But after I had calmed down and the week had passed I felt in a mentally strong place to cope with the upcoming operation.
Day Before Operation
I was first on the list on the Tuesday morning, so my husband Simon and I drove up to London the day before for the pre-op meetings. Mr Austin went through the operation and I signed the consent form. Alex took more pre-op blood tests including bloods for genetic testing (this had not been done before as my clinical diagnosis of Marfan Syndrome was made in the 1980s before the fibrillin-1 gene had been identified). I was given Hibiscrub to shower in (which made me smile as I use this for my cattle and horses!) and we were shown to our overnight accommodation. That evening was most surreal – walking past the London Eye, all lit up, and eating a meal overlooking the same. I was surprised at how calm I was (perhaps the Diazepam had taken effect!?) and thinking how strange it was to be out for a meal in London (I’m a country lass).
Operation Day: Tuesday 4 February 2020
We didn’t have a good night’s sleep, being woken by sirens all night long (!) and arrived back at the pre-op ward by 6.30am. Once again I found myself in a very calm state and thinking that this was all rather surreal. However, that was short-lived when the Anaesthetist Georgina came to talk to me – it all became rather real and I became scared and tearful. I was given Temazepam to help settle me and after a short while a nurse escorted us to the theatre doors. I can remember tearfully waving goodbye to Simon through the glass. There were several people in the room and I remember hot air being blown into a special blanket on the trolley bed (which was lovely as I feel the cold easily) … and talking a lot about my cows, dogs and horses. I don’t remember the cannulation at all, so the Emla cream worked wonders.
The operation went well and my personalised ‘jacket’ was fitted around my root and ascending aorta by the expert surgeon Mr Austin. I did suffer postoperative hypothermia so I remained on the ventilator for 11 hours whilst I was warmed up by the hot air blanket and my body temperature returned to normal. I remember responding to Simon’s voice when he visited for the second time about 6pm that day. The ventilator tubes were removed some time after that, which I remember (as instructions were being given to a trainee nurse during the procedure), but wasn’t unpleasant. I remained in Intensive Recovery overnight where I was closely monitored. At one point I felt sick, but was immediately given an anti-emetic drug which stopped it. The effect of the operation had a significant impact on my M.E. symptoms. My limbs felt like lead and I couldn’t move, just able to open my eyes and open my mouth a little for the nurse to feed me ice cubes, which helped my dry mouth.
Day 2: Wednesday 5 February
The next day I was moved to the High Dependency Unit. Whilst other patients were able to mobilise into a chair, I was still too weak to do so and my limbs still felt like lead, but a lovely nurse hand fed me soup, which was lovely.
Day 3: Thursday 6 February
On Day 3 I was helped into a chair and my chest drain was taken out, which was rather painful, but aided by the patient-controlled analgesia (PCA) Fentanyl. My catheter was also removed and I was transferred to the Doulton Cardiac Ward and later taken for x-ray. My Austin visited and showed me the video of my heart with its new ‘jacket’ fitted, which was fascinating and very impressive.
Day 4: Friday 7 February
Overnight my temperature spiked and after a blood test, ECG and Echocardiogram it revealed that I had Pericarditis (inflammation of the sac that surrounds the heart), which was treated with Ibuprofen and monitored. The cannula that was administering background pain relief and PCA was removed and I was given regular oral pain killers. The central line in my neck was removed, which was uncomfortable, but meant I was able to move my head a little easier. The dressing on my chest wound was also removed revealing a long, neat scar. That afternoon I was visited by Tal Golesworthy and it was great to talk to him about this innovative operation. He told me that I was patient number 299 in the world – amazing.
Days 5-8 : Saturday 8 – Tuesday 11 February
I struggled to cope without the intravenous pain relief overnight and the exhaustion and weakness were severe, so I became quite tearful. I was seen by the Doctors the next day and was told I should be medically fit to go home in two days’ time! That weekend was a particularly low point. Despite looking well and my heart progressing in the right direction after the operation, I was still unable to sit up unaided nor walk unassisted and without considerable pain in my legs and calf muscles. Although it is common for the legs to swell a little after cardiac surgery, it was alarming to see my usually skinny ankles and bony feet swollen to twice their size! On Sunday afternoon I was visited by the Physio who helped me walk using a walking frame and gave me exercises to aid my calf muscles. By chance I spoke to the lovely Matron Donna whose nursing friend had M.E. and she knew first-hand how debilitating the condition is and kindly had a word with the ACHD team. On the Doctor round the next morning (Monday) we discussed moving my discharge date back a few days to allow me to get stronger and to improve my mobility to a point where I felt safe to go home. As someone who suffers with chronic fatigue I am normally ‘Queen of Sleep’, but strangely for three nights I suffered with insomnia! I used that time wisely to do my exercises and practice my walking whilst the ward was quiet.
Discharge Day – Day 9: Wednesday 12 February
After surgery I had noticed that my vision was poor and I struggled to read the hospital menu card. Later I experienced aura disturbance so I was referred to the Emergency Eye Doctor. Images were taken and my eyes examined, which revealed nothing abnormal. I was told that I may have experienced an effective lens position change after surgery and the aura was put down to exhaustion.
After 9 days in hospital I felt strong enough to go home. My pulse was still raised (over 100 bpm) and there was still evidence of pericarditis, but I was told that these would improve with time. A discharge letter was actioned and I was given pain relief medicine by Pharmacy and left St Thomas’ at 6pm.
Clutching a rolled up towel to my chest I was driven gently home by Simon (a 2-hour journey south). It was lovely to be greeted by our Labradors, who sensed something different and were very gentle with me. Even with the awkwardness of sleeping propped up in a sitting position (it is advised not to lie on your side for 6 weeks whilst the sternum heals) I had a good night sleep in my own bed. It was also lovely to wake up and look out of the window at my little Dexter cows … a rather more familiar and comforting view than looking at the River Thames, Big Ben and the Houses of Parliament from my hospital bed, which was very surreal!
Day 13: Sunday 16 February
I still felt extremely weak and exhausted, mobilising just enough to get from settee to toilet, feeling dizzy and unbalanced. I was told that I may become more aware of my heartbeat after surgery (as the pericardium sac had been opened), but this would pass in time. After 4 days at home I suddenly became very aware that my heart was pounding and ‘jumping about within my upper body’ from my chest to my stomach. Our finger pulse oximeter showed my pulse bouncing about rapidly between 100 and 160 bpm and my blood pressure had soared, so after a call to 111 we were told to go straight to A&E. It was all rather scary, but I was seen straight away at Worthing Hospital and immediately wired up to heart monitors. The Atrial Fibrillation that I was experiencing was controlled by taking 2.5mg of Bisoprolol and I was kept in and monitored for 24 hours. I was told that this sometimes happens after heart surgery, but thankfully I did not experience another extreme episode, although did suffer some mild occurrences in the days following. I was advised to stay on a low dose of Bisoprolol (1.25mg) until my cardiac review at 6 weeks.
Weeks 3-6
The pains in my calf muscles subsided and I was able to mobilise much better. By week 5 I had the energy to get dressed and started short walks outside. I was still suffering pericarditis symptoms, with sharp pains in my chest, particularly when lying down or breathing deeply. I was also experiencing several temperature spikes. A blood test at my Doctor’s surgery revealed I still had some inflammation so I spoke to the Cardiac team at St Thomas’ and they advised an Echocardiogram, if I could get up to London the next day.
By now it was mid-March and Coronavirus was starting to affect the country with all out-patient appointments cancelled, including my upcoming 6-week Cardiac follow-up with the Surgeon, which would now be a telephone appointment. Able to access the hospital just before lockdown, my Echocardiogram showed that there was no more fluid around my heart, which was good news. As I mobilised more the pericarditis symptoms subsided and I was left with just the normal musculoskeletal pain in my upper body, which was manageable.
Week 8
At week 8 I started my Cardiac Rehabilitation. As the country was now in lockdown with Coronavirus I was unable to attend a class, so I was sent a Heart App with lots of information and Cardiac Exercises at different levels. This suited me well as I could work at my own pace and select exercises more tailored to my needs. Dedicated to the cardiac exercises and regular walking I became stronger and by week 10 felt more like me.
Post Surgery
I can’t quite believe that this has all taken place, but the long, neat scar on my chest reminds me that it has! I cannot praise highly enough the care and support I have received from Guy’s and St Thomas’. I feel privileged to have had this pioneering PEARS surgery, which was offered to me because I had Marfan Syndrome and I had lost my sister to aortic dissection just two years earlier. My journey may have been different to the standard PEARS patient due to my comorbidities, but it was a good journey and I would recommend it to others without hesitation.