My name is Andy.
I am 45 years old and work in management consulting, I am married, have two children and love to travel and play sports. A few years ago after a routine medical check up and scan of my heart, I was diagnosed with a dilated ascending aorta. After further scans it measured around 50mm which was outside of the normal range given my height of 196cm. Initially, they suspected this was result of Marfans, however, after going through the various tests and genetic screenings this was ruled out. Yet what they found was I had mutated one of my genes that they believe caused the dilation… well done me!
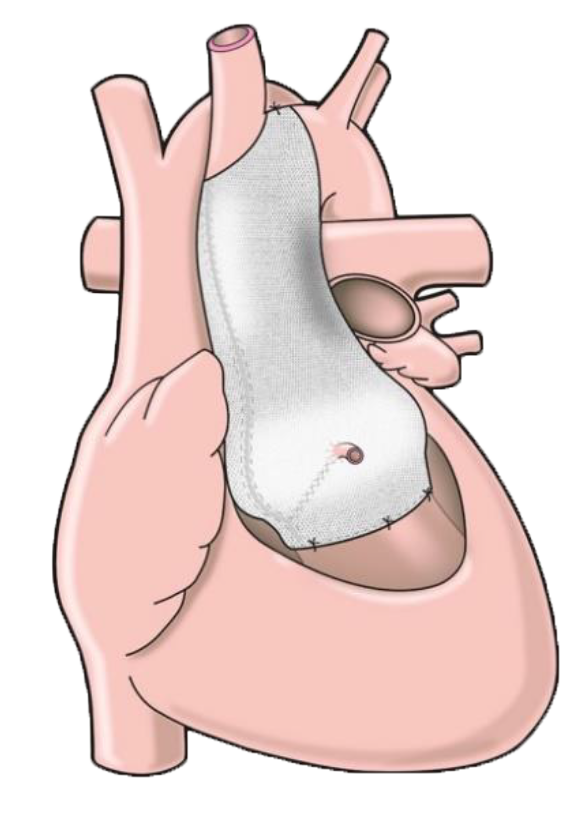
I spoke with a number of consultants over the next few months and years, who kindly talked me through the implications and risks of doing nothing over time, and the two available procedures to correct the dilated aorta. It was clear to me the outcomes of both would solve my problem, and the need for an operation was a ‘when’ not an ‘if’. The PEARS procedure, however, felt clearly advantageous to me, both in terms of the operation itself, and the fact that it left me ‘intact’ inside. Its innovative approach also appealed to my forward-thinking, progressive nature. The diameter of the ascending aorta over the next few years did not really change, however, given its size and potential to grow over time, I took the decision to have the PEARS operation at the Royal Brompton in London with Dr Hoschtitzky in order to move on with my life and remove this constant cloud of uncertainty. After further open and friendly discussions with the Dr Hoschtitzky about the procedure, its benefits and risks, along with reading all the patient stories on this website, I was ready for the operation.
Day 0: Monday 6 January 2020
Time to ‘check-in’ to my hospital hotel at Royal Brompton for the week. Very strange feeling so fit, healthy and going about your day as you have the last number of years, but knowing tomorrow afternoon you will be in intensive care.
I arrived 2pm and had the usual tests of blood pressure, ECG etc. then met with the doctor for a general check up to make sure I was fit for surgery – all good, all fine – cleared for take off. I checked into the ward at 4pm ish where I would hopefully be sleeping the night. Dr Hoschtitzky and the Anaesthetist came around to check up on me later that evening and talked me through what would happen again the next day. Yet again he reminds me that this will hurt and it will feel like I have been hit by a bus! … my expectations were fully managed.
I would be first on the list at 8:30 in the morning, with surgery planned for 9am, so no eating after 12am but some water etc. would be fine… no breakfast then. The Anaesthetist then asked if I would like a sedative in the morning to help me relax before I went into the prep room. I was feeling calm, but after asking a few questions, it didn’t seem like there was any downside to the tablet so signed up for it. My only other advice I would give at this stage is to go and have a nice meal outside the hospital to take your mind outside that environment – my wife and I did, and I returned to the ward for 9pm, ready to try and get some sleep. Before lights out, the Nurse came around with an electric shaver. Apparently I had to shave my whole chest… she advised me to also do my wrists where they put in other tubes which was a good tip. This is worth doing well as there a lot of sticky things on you whilst in hospital, so take your time shaving to make sure you are as smooth as possible!
Day 1: Tuesday 7 January 2020
Show time. Slept ok, as much as you can do in a ward, showered again using the special soap they give you and had some water… it’s now a waiting game. On schedule they come around with the sedative at 8am, then 8:30 am is time to get on the bed and go into the prep room (i.e. where they give you the general anaesthetic ) … very strange saying ‘see you later’ to my wife but feeling calm as I know what is going to happen the next few days and I know I am in good hands. I try and see if I can make the 10 count with the anaesthetic… don’t think I got to 4… that’s all I remember.
My eyes open, much like waking up in the morning… am in my gown in a bed, that’s good, then a hello from the nurse and a how are you and I quickly realise I am in the ICU… she says your wife is on the phone would you like to say hello… (She called her for me.) I get a few words out and am a bit dazed and explain I had just woken up, but do come and visit! My throat is very dry, so have some water and then tea… ahhh much better… then take in my surroundings. I am in a ward with 3 other people, each with our own nurse by our side. Feel ok, no pain, have a quick peek at my chest and see the honeycomb plaster taped on… not so bad or big as I thought. I have a line in my neck which is strange and one in my arm, ECG stickers on my chest then 3 tubes from my stomach… these are your drains I am told, they go into three separate water type bottles to collect any residue from the operation.
Have my first visitors and the anaesthetic and morphine is still flowing through my body so feel pretty good, no pain and able to talk (dry throat though) but don’t fancy moving. After a few hours I realise I need the toilet and am about to go as assume I have some sort of catheter in but think I should ask the nurse first…good job I did, no catheter she says… and passes me a cardboard bed pan/bottle… phew that was close. Food menu ordering time… all sounds fine but have no idea what I can stomach, but tick all the boxes as required….such a shame as when it comes all I can manage is half a banana and a bit of yoghurt. After that then a pattern of sleep, awake for some readings by the nurse, then sleep again for a little while… don’t remember too much more than that. A similar pattern follows in the night.
Day 2: Wednesday 8 January
Usual breakfast, some tea, a few bites of banana and a tiny bit of yoghurt… drinking a lot of cold water which is good apparently and does make me feel better. They do morning checks and then they are happy I can move to the HDU later that day, but first the nurse suggests the impossible-sounding task of getting out of bed and sitting in a chair… hmmm. She is right though, this is possible and slowly but surely I make it… that feels different, but good to be out of the bed… tired again though. Few hours later, back in the bed and they wheel me around to HDU… 3 other people in the room with me and two nurses this time. Pretty much the same routine; various biomarker tests, bit of sleep, lots of water, no big appetite. Sleep is hospital-like… i.e. a few hours here and there, nothing substantial but morning comes around.
Day 3: Thursday 9 January
I ate a whole banana for breakfast and a little toast… feeling slightly better. After the rounds the schedule for the day is to move me to the ward… hurrah. They do a chest x-ray on me with the mobile unit whilst in bed, my temperature is slightly high but comes down after some paracetamol… it is very hot though in the ward which they do acknowledge. To be allowed to move to the ward though I need to pass the walking test… I give it a go and walk to the bathroom and use it, then back to the chair next to my bed… Phew – made it – but know I can walk now even with all these pipes and things stuck in me, which gives me a good sense of progress.
The Doctor confirms I can go to the ward but they need to remove 2 of the 3 drains… they give me a 30 min warning and suggest I keep clicking the automatic morphine button. I have been using it here and there, but as no real pain I have been quite frugal in its usage, but I take this advice and keep clicking for the next 30 minutes. My advice is do keep clicking, as it is very uncomfortable when they take them out, so the more morphine in you the better. They come out, I am full of morphine and fall quickly into the deepest sleep for a few hours since I arrived.
A couple of hours later it’s time to be wheeled around to the ward… room with 5 other people, although two beds empty and one nurse for us all. Have some dinner, still not great appetite but eating slightly more… what I do actually eat is different from what I think I can stomach when I order. Feeling braver so I decide it is time to go to the bathroom and brush my teeth… slowly but surely and with help I manage it… back to the chair next to the bed to try and sit up and help the diaphragm… deep breathing helps as well, to avoid any lung infections.
By evening a few more visitors, but feeling tired. I decide to wash my face, shave and do my teeth before bed with the help of my wife… the feeling of cold water on my face is sooooo good. Say my goodbyes to my wife and then read in my chair before lights out at 10pm. Stomach feels strange… or is it my whole insides… they look like they are moving and being moved around in a washing up bowl… hmm, the nurse comes and they see my ECG monitor shows an irregular heart beat… this feels very weird and slightly scary. Apparently I am in arrhythmia… i.e. irregular heart beat as a result of the op, I do remember now them telling me about this as a possible side effect but like most of them I had ignored it as a possibility at the time. Apparently 60-90%of people get this after heart surgery… your organs are very sensitive so when they move or touch them in surgery it can slightly bruise them and kick this off.
They put me on a drip for the next 12 hours with an anti-arrhythmia drug… it’s a slow process to feeling better, and feels like I am on a ship at sea in very rough waters and have a sea sick feeling the rest of the night… needless to say I did not sleep at all, but by morning it has calmed down somewhat… but I feel exhausted and at my lowest point so far. I thought I was doing well, but this feels like going backwards. I manage to eat a bit more of a meal today, but so tired so sleep a lot between visitors and have to sleep when they are here. Sleep, eat, rest in chair, walk to the bathroom… that’s pretty much the day gone.
Day 4: Friday 10 January
Feeling a bit more normal and manage a whole breakfast… in the chair for the day and trying to take short steps and walks on the ward every few hours. Need to go to the x ray dept. which is close… no porters with wheelchairs available so decide I can walk this with my drip and drain… glad it’s close but get there and back no problems. Later that day I go for an echo… that is a lot further and worth the wait for a wheelchair! Just need to have a CT scan now but they can’t fit me in on Saturday. The nurse changes the dressing which sounds like it will be painful, but really is quite simple, peels off and quick clean and all good. By evening I am having full meal and feeling a bit more normal, can move around a bit more with the various contraptions but starting to see light at the end of the tunnel, the anti-arrhythmia drip finishes and I switch to tablet form for next 6 weeks as you have to come off it slowly… fine with me, don’t want that happening again.
Day 5: Saturday 11 January
Need the final sign off from the CT scan then can potentially go home on Sunday. Manage to get a slot in the afternoon and get taken down in wheelchair… is the coldest room in the whole hospital and feels good. They ask me to lay flat on the CT table and put my hands above my head… surely that’s not possible I think, but yes, as always they are right, I can do that. Initial scan looks good… looking like home time Sunday.
Day 6: Sunday 12 January
Get the all clear to check out. They remove the plaster from my chest and take the final drain out (not that bad), cannula in my arm and finally the line in my neck… I am free! … now all I need is my pharmacy prescriptions, outpatient discharge letter and sign off from surgeon… that surprisingly moves quickly and I am free to go by 13:00! I order a taxi to pick me up at the hospital and 50 minutes later I am back at home after possibly the strangest week of my life… physically and mentally many ups and downs, but in hindsight it was only 5 days. Once at home after a few hours, I feel like I could sleep for a few days… I crash out into a very deep sleep but force myself awake for dinner. Strange but good to be back in my own bed that night… I keep checking for tubes and things in my neck out of habit but they are not there… manage to lay down flat and sleep but wake up a few times with a cold sweat, but I am home.
After two weeks I feel good, walking each day and appetite back to normal. I stop taking any paracetamol and just rest at home reading books, doing jigsaws and a taking a couple of walks each day. I am slowly getting stronger by the day. I am not allowed to lift anything heavier than half a kettle full of water for the next 8 weeks though. After five weeks, back to hospital for check up and things seem all fine, I am allowed to swim and use an exercise bike to help get back my fitness, no contact sports until after 3 months from the operation.
Overall what can seem a daunting prospect in terms of heart surgery is in hindsight just a strange 5 days of your life in return for a lifetime of normality. If you are thinking about the PEARS procedure, then once you decide it is a ‘when’ not an ‘if ‘, based on my experience, I can only reassure you that you made the right decision. Thanks Tal for the invention… amazing!