My name is Kathryn Baurley and I am a 48 year old single mum with two boys aged 16 and 18, all living in Cardiff. We all have Marfan Syndrome and I had the ExoVasc operation on Monday 23rd August 2010.
I was told that I had Marfan Syndrome approximately 18 years ago. My eldest son was diagnosed around the same time and my youngest son diagnosed after his birth. Two years following his Marfan diagnosis, my eldest son was also diagnosed with autism.
To be honest, as the boys have grown, our lives have been pretty full of hospital appointments. Like most mums I know, you may have a problem yourself, but if your child has any sort of difficulty, major or minor, you tend to forget your own and concentrate on theirs. I took the boys to their regular Marfan appointments and did the same for myself, but any implications of the latter were pushed to the back of my mind. One thing my cardiologist said early on that stuck in my head was that, the fitter I was, the better able I would be to recover from any heart surgery, so I have always exercised regularly. However, for the seven years prior to 2009, my aortic root measurement never changed much from 4.3 mm and I thought that nothing was ever going to happen.
In summer 2009 I was sent for an MRI scan, my last one having been 5 years previously. At the follow-up appointment in October I was told that my measurement had increased to 4.85mm and that I needed an operation. It was a bit of a shock!
I spent 2 months thinking about the operation and at Christmas shared the news with the boys. The boys’ Dad works abroad, so there was a lot of planning to do, to help both the boys and me through this.
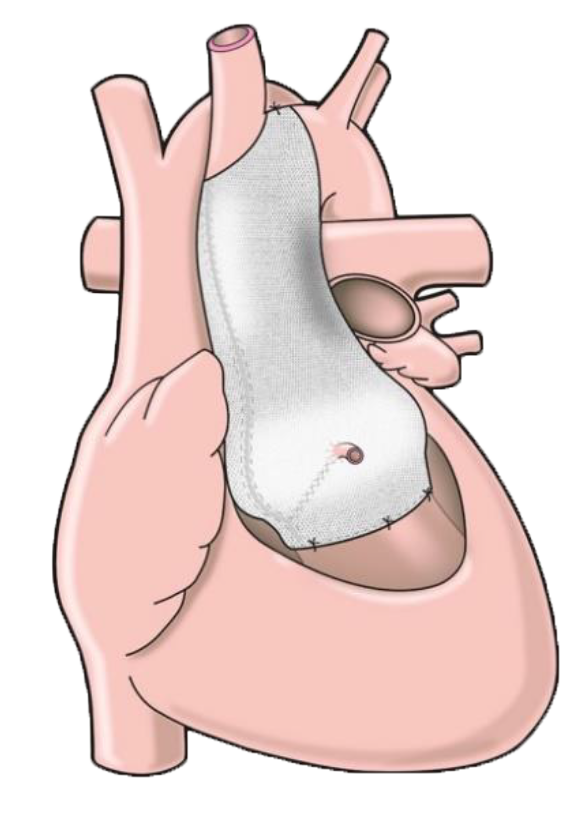
I had been told that I would see a heart surgeon at the local hospital in the spring. The appointment took place in March 2010 and a very likeable consultant told me all about the ‘Davids’ method. I told him that I had read about the ’PEARS’ method pioneered at the Royal Brompton, and wanted the chance to at least talk to the surgeon involved, Professor Pepper. This he agreed to, and in the meantime I read up on the subject and talked directly to Tal Golesworthy, which was quite an experience in itself! Although fully committed to his method, Tal openly answered the questions I gave him and then left me to see Professor Pepper and make my own mind up.
In May 2010, I went up to London to see Professor Pepper and I met up with Tal both before and after the appointment. After all the background reading I had done and after talking for only a very short time with the Professor, I was sure that this was the right method for both myself and my family. He agreed to wait until after the boys’ AS/GCSE exams that summer. Although this was still a huge, scary thing to me, the decision was made and I felt better.
The operation took place on Monday 23rd August after lots of planning and a lot of worrying. The boys and their Dad stayed in the hospital’s nurses’ accommodation, which was very basic and which they didn’t like much, but they were only there to sleep.
I don’t remember much of the day of the operation itself or the time in Intensive Care, apart from the shower you had to have before the operation. When I woke there was a cheery, chatty South African nurse who kept my mind occupied while I tried not to think about or look at the tubes coming out of me. The boys told me afterwards that their main concern had been the number of tubes coming from me (booklets had given a lower number). They found this hard to cope with (if you have younger children, then I would be wary of this), especially the one coming out of the jugular vein in my neck.
By day two I was in HDU (high dependency unit), where some tubes were removed, though not the one in my neck. Tal had warned me about the removal of the chest drains and they were a bit painful. Some air was left in my chest cavity during the removal of the drains, and I was checked daily by X-ray to ensure that the volume of air reduced, which it did.
Early on the Wednesday morning (day 3) I had an episode of arrhythmia (increased heart rate in my case) which is a common occurrence following any type of heart surgery. I had to have a 24 hour drip of a strong drug called amiodarone, followed by a six-week tablet course of the same medication, to which I had some horrible side effects. Despite this, I was up and walking with the physiotherapist the same afternoon (even with the drip) and walking on my own that evening.
The drip was removed on Thursday morning (day 4) and by the afternoon I had been moved to a normal ward (I would have been moved the previous day, but there was no bed available). The most wonderful thing about this was the shower I was allowed to have and I could put on my own clothes. I continued to walk (slowly) along the corridors and started to use the stairs too.
Every morning following the operation, between 6 and 7 am, Professor Pepper visited me and we had a relaxed, friendly chat. It was a sign of how human and kind he is: I felt like I was a person, not just a patient. I asked him on Thursday if it was possible to leave Friday afternoon (next day), as the boys were not happy and I felt that I was ready, to which he agreed, provided nothing changed medically and I had an echocardiogram (echo) before I left. The latter was ordered for Thursday afternoon, but was subsequently cancelled, and when Professor Pepper learned of this the following morning he went down to the echo department to ‘sort it out’ himself. I had the echo at 09:30 am, my package of medication by 1:30 pm and was in a taxi on the way to Paddington by 3 pm.
My recovery at home was better than expected, being fit before the operation was probably the main reason. However, I am a very bad patient and was trying to do things very soon after I was home. Once I could drive again after 6 weeks, things started to feel more normal, although I couldn’t lift heavy items and found the hoover difficult to use.
When all medical factors are equal and it’s a straight choice between the Davids/Bentall method or PEARS, there really isn’t any choice: the former requires hours more on the operating table, a lot of sewing and healing afterwards, heart and lung bypass, more pain and drugs and a longer recovery. The PEARS method has less of these worries, is shorter, less invasive and recovery should be shorter. Unfortunately, you can’t avoid going in through the chest wall, but the small size of the scar amazes everyone who sees it, it is so neat.
This isn’t to be taken lightly, but if you have reached this stage, then you haven’t got a choice: you have to have something done and the PEARS method just seems like the common sense option to me. You have got to check all the facts of both methods and talking to someone who has had the operation helps enormously and I am willing to talk to anyone who faces this choice in the future. It is early days yet, but I made the right decision.